The Emperor of All Maladies
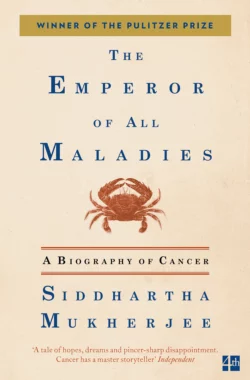
Siddhartha Mukherjee
Тип: электронная книга
Жанр: Зарубежная образовательная литература
Язык: на английском языке
Стоимость: 776.11 ₽
Статус: В продаже
Издательство: HarperCollins
Дата публикации: 16.04.2024
Отзывы: Пока нет Добавить отзыв
О книге: Winner of the Guardian First Book Award 2011Winner of the Pulitzer Prize for Non-fiction 2011Shortlisted for the Wellcome Trust Book PrizeShortlisted for the Duff Cooper PrizeNow, as cancer becomes an ever more universal experience, the need to understand it, and its treatment, has never been more compelling. In this groundbreaking and award-winning account Siddhartha Mukherjee tells the fascinating story of our relationship with this disease. From brutal early surgical treatments, to Sidney Farber’s hugely risky discovery of chemotherapy, to the author’s treatment of his own patients, he reveals how far we have come in solving one of science′s great mysteries and offers a fascinating glimpse of our future progress.