The Complete Blood, Sweat and Tea
Tom Reynolds
Collected in one volume, here are the true life stories of London ambulance driver, Tom Reynolds.*Previously published as Sirens, after the Channel 4 TV show inspired by the book*On any given day Tom Reynolds might be attacked by strangers, sworn at by motorists, puked on, covered in blood and other much more unpleasant substances. He could help to deliver a baby in the morning and witness the last moments of a dying man in the afternoon. He deals with road accidents, knife attacks, domestic violence, drug overdoses, neglect and suffering.And you think you’re having a bad day at work?His experiences spawned two volumes of memoir, both of which are collected here.
Sirens
Tom Reynolds
This book is dedicated to my mum and my brother, who have tolerated me with astonishing patience and love for almost forty years. It is also dedicated to all my work colleagues in the London Ambulance Service who do their best for the people who call them under some very difficult situations.
Finally to anyone and everyone who works for any of the emergency services – those people who bring calm to chaos, peace to despair and aid to the injured and frightened while working under incredible pressure and yet who rarely get the thanks that they deserve.
Contents
Prologue: Too Young
Part 1
Part 2
End Credits
Acknowledgements
About the Author
Copyright
About the Publisher
Sirens is not authorized or endorsed by the London Ambulance Service. The opinions expressed in this book are those of the author alone and do not necessarily reflect those of the London Ambulance Service.
There are a number of terms found in this book that may be unfamiliar; for the assistance of the non-medical reader there is a short glossary at the back.
In the interests of confidentiality patients have been made anonymous and identifying characteristics may have been altered or removed.
Read more at http://randomreality.blogware.com
Prologue: Too Young
Yesterday started well, we had the only new ‘yellow’ vehicle on the complex, and it really is an improvement on the old motors. But then we got a job that should have been routine, but unfortunately was not.
We were given a ‘34-year-old male, seizure’ at a nearby football pitch in the middle of a park. Also leaving from our station was the FRU (a fast car designed to get to a scene before the ambulance). As we had a new motor, we were able to keep up with the FRU.
Arriving at the top of the street, we were met and directed by some of the patient’s football team-mates. Unfortunately, the patient was 200 yards into the park, and there was no way we were going to get the ambulance onto the field – the council had built a little moat around the park to stop joyriders tearing up the grass in their stolen cars.
The FRU paramedic had reached the patient first and I ran across the field to get to the patient as the paramedic looked worried, and this isn’t someone who normally worries.
As I reached the patient, carrying the scoop which we would use to move him, the paramedic asked me if I thought the patient was breathing.
The patient was Nigerian, and it is not racist to say that sometimes detecting signs of life on a black person is harder than if the patient is Caucasian. White people tend to look dead; black people often just look unconscious. Also, a windy playing field at dusk is not the ideal circumstance to assess a patient.
‘He’s not breathing,’ I told the paramedic, just as my crewmate reached us. ‘Shit’ replied the paramedic, ‘I left the FR2
(#litres_trial_promo) in my car’.
I had to run 200 yards back to our ambulance to get this, now vital, piece of kit.
On my return my colleagues had started to ‘bag’ the patient (this means using equipment to ‘breathe for’ the patient and performing cardiopulmonary resuscitation, or CPR), which is the procedure to keep blood flowing around the body in the absence of a pulse. Attaching the defib pads I saw that the patient was in ‘fine VF’ (ventricular fibrillation) – this is a heart rhythm which means the heart is ‘quivering’ rather than pumping blood around the body to the brain and other vital organs. Technically, the patient is dead and without immediate treatment, they will remain dead.
We ‘shocked’ the patient once and his heart rhythm changed. It changed to asystole (this means that the heart is not moving at all, and it is much more difficult to restore life to the patient with this form of rhythm). We decided to ‘scoop and run’ to the nearest hospital. The paramedic secured the patient’s airway by passing a tube down the windpipe, and we got the patient onto the scoop, all the time continuing the CPR and giving potentially lifesaving drugs. We then carried him, with the help of his team-mates, to the ambulance and rushed him to hospital.
Unfortunately, the patient never regained consciousness, and died in the resuscitation room.
Thirty-four years old, normally fit and healthy – and he drops dead on a football pitch. Despite our best efforts there was nothing more we could have done for him; the treatment went according to plan and the resuscitation attempt went smoothly. This was a ‘proper’ job, but one job we would have happily done without.
PART 1
Why Won’t They Let Me Do This?
Here is a moan about something that I am not allowed to do. I’m not allowed to run people over in my job. I could really clear the streets of a lot of stupid people if I was able to do that.
Picture the scene: there I am, driving through the streets of London in a big white van, with blue flashing lights, loud sirens running and the word Ambulance written in rather large letters. As a pedestrian, what would you do? Would you think ‘Hmm, being run over by that would really hurt, I think I’ll wait the 12 nanoseconds that it takes him to drive past before I cross the road’. Or would you, as most of the people in my area apparently do, think ‘Hmm, an ambulance on his way to an important job, I bet I can run across the road in front of him before he can hit me’.
During the last job, three people tried to dive under my ambulance. If I was allowed (by government grant or some such) to keep driving and splat them across my windscreen, that would mean three less idiots being allowed to breed tonight.
Oh well, I might get lucky later tonight.
Dear Mr Alcoholic
… Can all alcoholics please just get drunk in their houses and fall asleep there? Why do you insist that you drink your Tennent’s Super in a public place where some do-gooder will think you are ill and call for an ambulance?
… Can you also have a bath once in a while? I know it’s nice to roll around in the road while drunk, but it would be nice if you were at least a bit clean to start with.
… Would you mind awfully not swearing at me, taking a swing at me or exposing yourself to me? I have quite enough abuse from the non-drunks out there … Still at least your fists are easy to dodge, and if I stop holding you up, you fall over.
… If you have a medical condition, please don’t use it as an excuse to get taken into hospital. If you tell me ‘I’m drunk and need to sleep it off’, I have less work to do than if you tell me that you have ‘Chest pain, Angina, Cancer and Difficulty in Breathing’. The more tests I have to do the longer it will be before you get to hospital, and the more I have to come into physical contact with you. If you are just drunk, then I can just be a taxi.
… When you have been sick, at some point in the next week or so could you please change your clothing? Give them to someone who hasn’t knackered their brain on booze to wash. Dry vomit on the clothing, while advertising your love for beer, doesn’t endear you to me thankyouverymuch.
… Please keep your weight down either through diet or through terminal liver failure. I’m the poor bastard that has to lug the dead weight of your unconscious body into the ambulance.
… You don’t have to tell me ‘I’m an alcoholic’, and sound so proud about it. I do have a nose, and can smell for myself.
… Finally, although Tennent’s Super Strong lager, White Lightning, and for the rare rich alcoholic Stella Artois are perfectly acceptable drinks, could you please come up with something less damaging? I think lighter fuel is better for you and contains fewer chemicals.
A Child is Born …
The story of the first baby I delivered – I can still remember it now. I can also remember my feeling of relief when it all went smoothly. Yet still managed to turn it into a rant about midwifery.
Just in from my late-shift and feeling more upbeat than normal. Tonight I delivered my first baby … and yet I can still turn this happy event into a rant.
Picture the scene: you are a midwife (this means you have a chip on your shoulder the size of the African debt), and a lady comes in to your maternity department in the second stage of labour. Do you …
(a) Say hello, take a room and we’ll have that baby out as soon as we can,
or …
(b) Tell them to go home and come back when the pain gets worse.
Guess which answer results in your baby being delivered by an ambulance bloke who has 1 day’s training in maternity (and who, to be honest, slept through most of it)?
Then when I take mother and baby into the same maternity department are you …
(a) Vaguely apologetic, or …
(b) Snotty towards the ambulance crew who did your work for you?
Can you guess that tonight I got (b) for both questions?
Otherwise it was a nice simple delivery, with dad shooting pictures on his mobile phone sending them to all and sundry while his wife was lying, bloodstained and naked on a leather sofa. Blood went all over that sofa, which come summer will start to smell just a little rank. Blood also went all over me (note to self – must remember to pack Wellington boots next time) and my acting skills (‘Don’t worry mum, all normal, I’ve done hundreds of deliveries’) were tested to the limit.
… and I didn’t have to pick up any alcoholics.
Why Would People Even Think It?
I have sometimes been astounded by the bloodymindedness of people, and sometimes by their stupidity. Now I am astonished at their petty nastiness.
I’m driving my ‘big-white-van-with-blue-flashing-lights-and-a-siren’ to a 1-year-old child with difficulty in breathing. While passing a group of youths on the pavement, one of them thinks that it would be a good idea to throw his bottle of coke at the ambulance, thus spraying my screen, obscuring my vision and nearly causing me to swerve into oncoming traffic.
All I can say is that it is lucky for them that I was going to a call, because if I hadn’t I’d have shoved my boot up their arse.
Where in the tiny recesses of their minds does it seem like a good idea to throw something at an ambulance running on lights and sirens?
All I hope is that one day they need me – something likely, given the amount of people like that who get stabbed in my neck of the woods – and I’m just that little too slow to save their worthless skins.
Payment Point
I get called to a lot of RTAs (that is, for the uninformed, ‘Road Traffic Accident’). I’d say that 90% of these are diagnosed as ‘whiplash’ (which is a muscular sprain of the neck – this is a minor injury that is treated with painkillers); I’d suggest that over half of these are an attempt to gain insurance money. In the ambulance trade we call this the ‘Payment Point’, referring to the point in the neck that is painful, and pays out the money.
Tonight I saw the most blatant attempt to get money from an ‘accident’.
I was called to a flyover where two cars had been in a near collision, yes, a near collision. There was no damage to either vehicle, neither were there any skidmarks on the road. The ‘patient’ was the passenger of the car, and complained of pain on the right side of his neck. He was desperate to go to hospital, for what reason I did not know, as there was obviously no injury.
This was made even more evident when he forgot what side of his neck the pain was on. When I called him on this he pretended not to know what I was talking about.
Even the police were not above making fun of this idiot.
It probably didn’t help that he was 10 years younger than me and cruising around in a red sports car.
Of course RTA is now RTC (Road Traffic Collision), because if it’s an ‘accident’ then the police can’t prosecute anyone.
Single
Although I do love my job dearly, there are a number of disadvantages. At the moment I am a ‘relief’ worker, which means although I have a main station, I can be sent anywhere in London to cover absences and holidays in the ‘Core’ staff. I also don’t have a regular crewmate … I am essentially the whore of the London Ambulance Service.
So, at the moment I am sitting on my backside at my main station with no-one to work with, watching daytime TV.
Bored, Bored, Bored, Bored …
Of course, at some point in the next 12 hours I could be rushing off anywhere in London. Being on strange stations is actually quite good fun, as you get to meet new people and, let’s face it, in this job moving around London just means ‘same shit, different scenery’.
… But at the moment I’m bored …
Daytime TV, the ambulance relief’s worst enemy. Thankfully I’m no longer a relief – I’m ‘Core’ staff now, which means I have a regular partner and I work mainly out of one station.
Some People Just Can’t Wait
So, there I am in my ambulance helping a bloke who was actually quite ill, when all of a sudden the back doors fly open and some idiot decides to start berating me because I’m blocking the road. Needless to say I am not pleased at this, not only because it is embarrassing for the patient, but also because of the sheer bloody cheek of this person. When I tell her (very politely mind you) to bugger off, she replies with the old favourite ‘I’m a taxpayer and I pay your wages’. At this I remind her that my patient, my crewmate and I also pay taxes. At this she is a bit nonplussed, yet still she continues to moan that there is no need for me to block the road.
In any event, I did need to block the road, I don’t do it on purpose, but it is more important to get to the patient quickly.
This woman’s moaning then gets other drivers upset and they start honking their horns, and the only way I get rid of the woman who was in such a hurry was to pull the door shut after me and tell her to imagine her relative in the ambulance …
I didn’t hurry treating the patient either.
The same thing has happened on more than one occasion. Now I simply ask the complainer that if it was them rolling around in agony, would they like to have to wait while I find a better place to park?
Maybe it’s Because I’m a Londoner
Research carried out by the London Ambulance Service for our ‘No Send’ policy has shown that 59% of Londoners think that they will get seen quicker in A&E (Accident and Emergency department) if they arrive in an ambulance.
This … Is … Not … True …
In fact, if you come to A&E after calling an ambulance for something minor, the nursing staff will be more inclined to send you out to the waiting room and forget about you.
I was an A&E nurse for a long time – just trust me on this …
Also, Londoners call for three times the number of ambulances for ’flu than in any other English city. Half the time the patient has got a cold and not ’flu at all, and just needs to work it out of their system. Even if they did have ’flu, there is little the hospital could do for them anyway.
Coupled with high population densities, lack of staff and vehicles, speed-bumps everywhere and heavy traffic, is it any wonder we are having trouble hitting the 8-minute deadline we have to make 75% of calls in?
Nice New Motors
The London Ambulance Service is giving us poor ambulance staff shiny new ambos to drive … well, puke yellow rather than shiny … but they are new. These are Mercedes Sprinters outfitted in ‘EURO RAL 1016 Yellow’ which is apparently the most striking colour available and is used throughout the European Union. They have lots of nice new bits for us to play with. Most importantly, they have a tail lift so now we don’t need to break our backs lifting some 20-stone lump into the back of the motor (20 stone is 127 kilograms for those using ‘new money’).
I was asked by a friend what I thought of them, and having just finished my ‘Familiarisation Course’ (4 hours of playing with the new toy) I must say I do like it. Not only is the engine more responsive when moving off, but the brakes also work that bit better than our old LDVs (Leyland Daf vans) and the interior is much more professional looking.
The only real problem I foresee is that the tail lift needs around 4 yards to unload the trolley and around London this means that we will have to park in the middle of the road, blocking off other traffic. So, if you do see one of us blocking your way, please realise that there is no way we can park the things and be sure of being able to load a patient on board as well.
These things also cost £105 000 each and if we get the slightest scratch on them they have to be taken off the road and repaired (unlike the ones we have at the moment where they are beaten up until they stop working). Since our insurance has a £5 000 excess it’ll mean a lot more money going to vehicle maintenance.
Should be fun, but I can’t see management ever letting me drive one … I estimate if I can squeeze through gaps by driving until I hear the crunch …
While I thought that parking to allow the tail lifts space would be a big problem, our biggest problem would turn out to be the regular breaking down of the lifts.
My (So-Called) Exciting Life
I had my hair cut today, which has become a weighty decision in my mind. It goes something like this …
(a) Do I get a crop or not? If I get a crop I’ll look like I’ve just been released from a concentration camp; if I don’t then I’ll look like a paedophile.
(b) Will my mum like it? If not then I’ll have to put up with 3 weeks’ worth of moaning about how terrible I look.
(c) Will this cut enhance my ability to attract members of the opposite sex? To be honest, no haircut has ever done this but I live in hope.
(d) If I go to my local hairdressers will I get the trainee … and if I do will it be possible to get a refund?
Anyway, I went in and got a ‘short-back-and-sides’ and rather unfortunately I’m deaf as a post when I’m not wearing my glasses (for those who have 20/20 vision, you don’t wear your glasses when getting a haircut). So when the whole place erupted in fits of laughter I didn’t know if it was because of a rapidly growing bald-spot.
(Still while I can’t see it, it doesn’t exist.)
The best I can say is that I’m not having to brush my hair out of my eyes with a pair of gloves covered in someone else’s vomit.
Which is nice …
Bloody Cat …
I’m sitting here single on station (you need two people to man an ambulance, and if you haven’t got anyone to work with you are ‘single’ and therefore unable to work. However, you need to stay on station in case they find someone else in London who is single. In that case you find yourself trekking across London to work in a place you’ve only seen on telly). I’m hungry and bored, partly because it’s night-time, and partly because there is no-one else on station.
However I have a plan …
To counter the boredom I have a DVD I can watch on the station’s new DVD player (bought out of staff funds, so no we haven’t been defrauding the NHS). The hunger problem will soon be solved by the microwave curry I have sitting in my car.
Let us now introduce a new member into the cast: when I said I was alone that was a bit of a lie, there is the station cat. Well at least I think it’s a cat as it is so threadbare it could be anything. This cat is so stupid it lies in front of your ambulance just when you need it the most, and refuses to move until you physically have to kick lift it gently out of the way. However, it is intelligent enough to realise that when someone is using the microwave there will be an opportunity to beg for food 5 minutes later (13 minutes if the food is frozen).
I nearly fell over the damn thing stepping away from the microwave, only to spend the next 10 minutes discussing with a mouth full of chicken korma why it wouldn’t like to jump up on my lap and make off with my dinner. It went a little something like this …
Miaow.
‘No you can’t have any.’
Miaow.
‘You wouldn’t like it.’
Miaow.
‘Go eat your own dinner.’
Miaow.
Gets up, plate in hand, to check that the cat does indeed have food/water/toy mouse.
Miaow.
‘Will you bugger off!’
Miaow.
At this point I put the plate (still with some of my food on it) on the floor, which the mangy beast sniffs and turns his nose up at. Said ‘cat’ then goes and hides under a table.
Horrible bloody creature.
It’s now dead; there is only one person on station who misses the bloody thing.
Why This Is a Good Job
My crewmate and I went to a man having a fit on Christmas day; he was a security guard and built like a brick out-house. This fit wasn’t your ‘normal’ epileptic fit, but instead the man was punchy and aggressive. To say it was a struggle to get him on the back of the ambulance is to say that Paris Hilton may have appeared in an Internet video download. Cutting a long story short, the patient is diabetic and his blood sugar has dropped to a dangerously low level. Luckily, we carry an injection to reverse this, and after wrestling with him in order to give him this drug he made a full recovery before we even reached the hospital. This is a nice job because we actually helped someone rather than just drove them to hospital.
Other benefits of the job include (but are not limited to …)
Working outside in the fresh air. I don’t know how office workers put up with air conditioning.
For much of the time you are your own boss – do not underestimate this.
Driving on the wrong side of the road with blue lights and sirens going; it’s not about the speed it’s about the power.
Being able to poke around people’s houses and feel superior even though you haven’t done the washing up in your own house for 2 days.
No matter how annoying the patient is, knowing that within 20 minutes it’ll be the hospital’s problem.
Meeting lots of lovely nurses, and knowing that I get paid more than them.
On the rare occasion, being able to help people who are scared or in pain.
Every time I have a bad day, or feel fed up at work I think back to this list and soon start to feel better – although I no longer get paid more than the nurses I meet.
Death and What Follows
There are some people, who despite being lovely people, you dread working with; one such person is Nobby (not his real name). He is what is known in the trade as a ‘trauma magnet’. He’s one of those people who will get the cardiac arrests, car crashes, shootings and stabbings; by contrast I am a ‘shit magnet’, meaning I only seem to pick up people who don’t need an ambulance. Other than having to do some real work for a change I really enjoy working with him.
I was working with him a little time ago and we got called to a suspended (basically this is someone whose heart isn’t beating and they have stopped breathing). It’s one of those jobs that require us to work hard trying to save the punter’s life. We got to the address and found relatives performing CPR on their granny. You might have seen it on TV as a ‘Cardiac Arrest’.
(Let me correct a few ideas you might have about resuscitation. First, it rarely works; ‘Casualty’ and ‘ER’ have led people to believe that you often save people: I can count on the fingers of one hand the number of people who have survived an arrest and most of them arrested while I was watching them in hospital. Second, it isn’t pretty: when someone arrests there is often vomit, faeces, urine and blood covering them and the area around them. Finally, people never suspend where you can reach them: if there is an awkward hole, or they can find some way to collapse under a wardrobe they will do so.)
This poor woman was covered in body fluids and was properly dead; there was no way we were going to save her. One of our protocols says that we can recognise someone as beyond hope and not even commence a resuscitation attempt. Unfortunately, we couldn’t do it this time as the relatives had been doing CPR (which is the right thing to do) and so we had to make an attempt.
Nobby and I got to work and tried to resuscitate the patient for 30 minutes. Our protocol goes on to say that if we are unsuccessful after attempting a resuscitation for ‘a specified time’ we can end it and recognise death, which is what we did.
However, during our resuscitation attempt it seemed that the entire extended family had arrived and there were well over 20 people in this little terraced house with much wailing and gnashing of teeth. It’s always hard to tell someone that their mother has died, but it has to be done, and if you can manage it well you can answer some of their questions and hopefully provide some healing for them.
The GP (general practitioner) was informed, as were the police (a formality in sudden deaths). The family had called a priest and he was there before the police arrived, while the GP was going to ‘phone the family’; what he expected to be able to do over the phone puzzled me.
We tidied up and went onto another job.
Two weeks later, Nobby was called to a chest pain. He turns up and finds himself in the middle of a wake, surrounded by 20 familiar-looking people.
Can you guess who the wake was for? Its a funny old world …
I worked with Nobby again for the first time in 2 years. He still remembered the job, and what happened after it. I told Nobby that he’d be included in this book but he wasn’t happy with his pseudonym and told me that he would prefer to be referred to as ‘George Clooney’. I refused.
I Do Like Some Drivers …
Although I often moan about the idiocy of other people’s driving when faced with a big white van with blue flashing lights on top, I am sometimes pleasantly surprised at the lengths some people will go to in order to get out of the way. For example, yesterday we had people nearly grounding their cars on roundabouts and roadside verges, squeezing into parking spots I wouldn’t be able to fit a Mini Cooper in and swearing at other drivers who wouldn’t move out of the way. I’ve had workmen stand in the middle of the road and stop traffic, lollipop ladies fence off crossings with their ‘lollipops’, and van drivers who I have clipped while squeezing past them wave me on and tell me, ‘don’t worry about a little damage’.
Yesterday we had all the above on one call (except hitting a van driver), it was like the Red Sea parting before us. It was a beautiful thing to behold; it left us in awe and wonder.
Shame we were going to 2-year-old with a cough.
This is a rare occurrence.
The Dangers of Prostitution
Occasionally you get a job that makes you laugh, normally because the person you are picking up is an idiot. We got called to a chip shop in one of the main roads in Newham – unfortunately there are about 20 chip shops on this road, but we managed to narrow it down by looking for the shiny white police car parked outside. The call had been given as an ‘assault’ which can mean anything from a slap on the face to a fatal stabbing.
In this instance it was a young lad, the spitting image of ‘Ali G’, who was complaining that he had been hit on the nose; needless to say there wasn’t a mark on him, and it turned out that he had been hit by his girlfriend. The police wanted to take statements, but he wasn’t interested and when I tried to assess him he told me that the ambulance wasn’t needed as ‘I’m St Johns innit, and a security guard’. This fella couldn’t scare a toddler, so I suspected he was telling a little bit of a lie. As he wasn’t hurt and ‘refused aid’ my crewmate and I retreated to a safe distance to do our paperwork …
In the course of the night we found ourselves at the local hospital (dropping off yet another ill person) when who should walk in with another crew from my station, but our earlier ‘Ali G’ lookalike. I asked him why he decided to call an ambulance when he’d already sent us packing and it turned out that another woman had hit him … the prostitute he’d hired after his girlfriend had slapped him. Turns out she had hit him and then robbed him of his jewellery. He couldn’t have put up much of a fight because he only had one scratch on him.
It’s pillocks like these we have to put up with … and call ‘sir’ …
However, it is also jobs like this that we can use to have a good laugh with our workmates. So people like him do serve some purpose.
My Night Shift
Much fun and games last night, working in the Poplar/Bow area. Not only did some German bloke graffiti on the back of one of the ambulances, but he also called the crew from a payphone and ran off, repeating it twice.
There are a lot of strange people out there …
MacMedic (an American ambulance blog) gave a rundown of what his shifts are like, so I thought I’d do the same, in honour of our brothers in foreign climes.
All these people called an ambulance last night by dialling ‘999’.
(a) Fractured wrist – young lad at the Boat Show.
(b) An alcoholic ‘frequent flyer’ who has just been released from prison … We thought we’d got rid of him for good.
(c) A 15-year-old with a runny nose.
(d) Very minor RTA.
(e) Domestic Assault, with no actual injury, but police already on scene.
(f) ‘Facial Injury’ which turned out to mean ‘Some bloke kicked my door.’
(g) Assault with a cut hand – actually a decent injury with tendon involvement (which means surgery and physiotherapy).
(h) Varicose Vein that had burst – plenty of blood everywhere.
(i) A 29-year-old with chest pain, hyperventilating, with very upset relatives.
(j) A suicidal overdose in a house filled with young men with short hair and tight T-shirts (ifyouknowwhatImean).
(k) RTA with a traffic light pole coming off the worse in a two-car collision.
(l) An 8-month pregnant female who had fallen earlier that day.
and …
(m) A fitting 9-year-old; only one parent spoke English, and they decided to stay at home and send the father who doesn’t speak English with us, because ‘The hospital has interpreters …’
Now, out of these thirteen jobs, only five actually went to hospital …
This counts as a ‘good shift’, reasonably interesting jobs, and no-one tried to hit me.
I Hate Psychiatric ‘Services’
Sorry folks, bit of a rant here … but I last slept 22 hours ago …
We got a call to a patient who was ‘Depressed – not moving’: normally with this type of call it’s some teenager having a strop, but this time it was a little different. Basically, the patient, who suffers from depression, was discharged from the local psychiatric unit 3 weeks ago and recently had her dose of antidepressants reduced. Yesterday, she was crying all night, and tonight she was just sitting staring into space, refusing to make eye contact and not talking at all.
One of the things that we as an ambulance crew cannot do is physically remove someone to hospital if they don’t want to go – that would be kidnapping and is frowned upon by the law. This young girl was not going anywhere despite my best attempts to persuade her – she just wasn’t communicating.
The solution would be simple: call the Community Psychiatric Nursing (CPN) team to come and assess her and, if needed, arrange her compulsory removal to the psychiatric unit (called a ‘Section’ under the Mental Health Act). The problem? It was 10 p.m. …
First off I phoned the psychiatric unit that she had received treatment under. After talking to two idiots who had trouble understanding plain English, I finally managed to get the number of the CPN team. Now, the London Ambulance Service (LAS) is quite smart: when we want to arrange an outside agency we go through our Control because all the telephone conversations are recorded … so if someone says they are going to attend they damn well better. I got onto Control, passed the details to them and waited for them to get back to us.
I’d just like to say that in all my years of medical experience I have never had a simple referral to a psychiatric service: they always seem to try shirking any form of work by ‘forgetting’ you or by being just plain obstructive. Maybe I’m just unlucky and get the idiots every time.
Needless to say we waited … and waited … and waited … from 22:20 until 23:00 we waited; then at 23:02 Control got back to us. Apparently the CPN team all goes home at 23:00 and hadn’t answered the phone until 23:00 on the dot. So they refused to visit the patient. The moral so far is if you are going to have a psychiatric breakdown in Newham don’t do it after 22:00.
So we switched to plan ‘B’, which is to arrange the out-of-hours social worker to come and visit, as they double as Psychiatric Liaison. Again we went through Control and waited … and waited … and waited … Finally we heard back that the social worker would ring the family and would like to talk to me. (Outside agencies try this trick, as they know the patient’s phone isn’t being recorded, and so can say whatever they want, with any disagreement being my word against theirs.) The social worker explained that she was very busy and so would prefer not to come to see the patient and have I tried the out-of-hours GP?
Back to Control I went and got them to try and contact the out-of-hours GP (a GP, for those not in the UK, is the patient’s family doctor). Can you guess what we then did? We waited … and waited … and waited … Finally, Control got back to us and informed us that the out-of-hours GP hadn’t arrived for work yet and that when they did, they would have to see two other patients first.
All through this time the family of the patient were very understanding and were happy when I explained that the GP would call at some point in the night. All I could do was advise them to remove anything that the patient could use to hurt herself, and keep an eye on her, calling us back if they felt the need.
Total amount of time an ambulance was tied up trying to get outside agencies to DO THEIR DAMN JOB – 2 hours and 19 minutes … and not the world’s most satisfactory outcome.
As I mentioned to our Control, sometimes you feel very lonely out there on the mean streets of Newham.
It is still the case that as soon as the sun goes down, various community services disappear and people in trouble need to rely on the ambulance service and the A&E department, even if it isn’t the best place for them.
Sticky Feet
There is something deeply disturbing about walking on a sticky carpet – especially when the flat is in a complete mess and the punter has called an ambulance 4 times in the last 2 days for a pain in the chest that has lasted 2 years. I’d like the jury to note that the pain hasn’t changed in any way, it’s not worse, or moved around the body, he has no other symptoms. But the patient just seems to like calling ambulances. I wanted to wipe my feet on the way out of the flat.
It also doesn’t help when the patient smells so bad that I want to leap out the side window. We didn’t have any air freshener (and apparently, neither does the hospital).
When we got to the hospital the triage nurse took one look at the patient, muttered ‘Not him again’ and sent him out to the waiting room. I suspect that it may just be a ploy to use biological warfare to empty the waiting room.
I still keep getting called back to him for the exact same ‘problem’.
Workload
Once again I know a lot of visitors here are from America, so I’m going to explain how the LAS works on a day-to-day basis. This will either be very boring or immensely interesting – your choice.
Ambulances run out of dedicated stations, we don’t share stations with the Fire Service. In fact, some years ago, when it was suggested the idea was shot down as we would be disturbing the firecrews’ sleep throughout the night. Each station has its own call-sign ‘K1’, ‘J2’, ‘G4’ for example, then each ambo has a suffix that is attached to this, so one ambulance running out of station J2 would be called J201, while another would be J207.
The stations are spaced approximately 5–6 miles apart, and you mainly service the area surrounding the station; however, with interhospital transfers and other irregularities you can quite easily find yourself across the other side of London.
It’s an old joke that when asking if we need to travel so far the dispatcher will ask us if it still says London on the side of the ambulance.
There is a main station, and two or three ‘satellite’ stations; the main station will normally have between three and six ambulances running from it, while the smaller stations have between one and four. There is less cover at night, and you can easily find yourself being the only ambulance running from a given station.
Across London we deal with more than 3 500 calls per day, and with a fleet of 400 ambulances of which perhaps only three-quarters are manned, we seldom get a rest. Where I work we average 1 job an hour, and are supposed to transport every one of those patients to hospital.
The longest shift we officially do is 12 hours, in which we can expect 10–13 jobs, which doesn’t sound like a lot but is enough to keep us busy … We spend 97% of our time away from station (compared with 3% for the fire service).
However, it is a fun job.
Night Shifts
There has been a discussion over on another medical blog’s forums over which shift we prefer to work. Like many of the others I have a preference for working through the night. The reasons for this are many but include:
(1) I’m single, I can lie in bed as long as I want. And breakfast is dinner … and kebabs are lunch … and an icecream is supper.
(2) You get empty streets, and so can drive like someone out of ‘The Fast and the Furious’.
(3) You also get the strange jobs: ‘sex-toy accidents’, criminal behaviour, stabbings … (4) It feels as if you ‘own’ the world: there is no-one else around, and anyone you do meet is normally shocked to be awake at night.
(5) You get to work a lot of jobs with the police, who are generally excellent people to work with.
(6) I get to sleep through early morning television – I’m sorry but I can’t see the attraction of ‘Trisha’ or ‘This Morning’.
(7) I don’t have to go into a school, and be surrounded by 400 screaming children just because a kid has sprained their ankle.
(8) There is less management around – actually there is no management around (always a good thing); I like to avoid management as much as I can: I worked this job for 6 months before they remembered my name.
(9) On a cold winter morning, I’m going home to my warm comfortable bed, while everyone else is trudging to work.
I still like nights, which makes me a rarity in the LAS. Most of my most interesting jobs occur at night.
Busy, Busy, Busy
No sooner do I post why I like night shifts than I get two ‘proper’ emergency calls, one after another. The first was a 76-year-old Male ‘Suspended’. Unfortunately, despite our best efforts there was little hope for him, and he died later in hospital without his heart ever restarting. His wife of 50 or more years was disbelieving of the whole situation, and I was too busy doing CPR to be able to comfort her much. It is one of the few things that I miss about nursing – sometimes you want to spend time with a relative. If you can’t do anything for the patient, the relatives then become your concern. For the first time in 50 years she was going to sleep alone and the nurse who would be looking after her is not someone that I would call the most sympathetic person in the world. I spent a little longer at hospital talking to the wife. The only consolation that I could give her was something that I’ve practised many times over the years – that her husband never suffered, and that he wouldn’t have felt anything that we did.
The next job was a man who, after drinking too much, fell over in the street. He had a greatly altered level of consciousness, possibly due to the alcohol but also possibly due to the large head injury which was leaking a frankly excessive amount of blood over the tarmac.
He could have been worse – he was lying in the middle of the road and could have easily been run over. It is important in such a job that you should ‘collar and board’ them. This is a way of immobilising someone in order to prevent any damage to the spinal cord. Unfortunately the patient was quite combative and so the only safe way to secure his head was for me to hold it during the transport – all the time blood was leaking through the dressing we had put on him, all over us, the trolley bed and the floor of the ambulance. Some managed to flick up onto my crewmate’s face, which is something you don’t really want happening to you.
I’ve just come back from the hospital (after dropping off yet another assault) and our patient is doing fine – seems that his altered consciousness was indeed as a result of the alcohol. He still isn’t sober enough to have a meaningful conversation, but he is looking a lot better than when we picked him up.
I still like wrestling with drunks, and writing about blood being flicked up into your face set the stage for a future set of posts.
New Uniforms (But Still Green)
The LAS has got some new uniforms. These include ‘combat trousers’ and a fleece, which is nice seeing as it can get a bit nippy around here. The only problem is that we use ‘Alexandra’, who doesn’t have the best reputation, for our uniforms. We’ll forget that they can’t measure you up correctly – I am not a 38-inch waist no matter how many kebabs I eat. Instead, let us consider that the buttons on their shirts tend to fall off at the worst possible moment. Having a button drop in a dead man’s mouth when you are trying to resuscitate him is not something that inspires confidence in the relatives watching. I was supposed to have eight shirts; two of them have been cannibalised, so that I have six shirts with the right number of buttons.
The new uniform actually seems quite nice. We have a little NHS logo in case the big motor with ‘Ambulance’ written on the side is not enough of a clue to our identity, and the shirts have a mesh in the armpits so we can let our sweat out. The combat trousers have ‘Permagard’ (their spelling, not mine) which is designed to kill bacteria, which is nice considering the state of some of the houses we visit. The high-visibility jackets are … well … visible and we now have a green ‘beanie hat’ (I think it’s green so that people won’t wear them anywhere except at work).
There is a rumour that we will be getting new boots soon … ‘Magnums’. We are a bit like the army in that we buy our own boots because the ones supplied are a bit shoddy.
Anyway the uniform ‘goes live’ on the 12th but those who have uniform that actually fits have been wearing them early. The bosses are moaning a bit but haven’t actually told anyone off about it.
I now have five shirts with the right number of buttons. People are still buying their own boots.
Daddy, Daughter, Kill
Picked up an assault yesterday. While sitting in the back of the ambulance he told his 2-year-old daughter that ‘daddy is gonna fucking kill the people who did this to me’, then complained when the nurse at the hospital told him to moderate his language.
I love this job.
We then went to someone who started hitting his own nose in order to prove that it had been bleeding earlier, and then went to a woman who had a bleeding varicose vein that had stopped bleeding, but wanted to pick at it to prove that it had been bleeding.
Then we went to a 14-year-old girl who was ‘fitting’ but when we got there was confused and combative – she was a diabetic so we checked her blood sugar, which was low. Being confused is one of the symptoms of a low blood sugar and we normally give them an injection that brings them out of it. We gave the injection and waited for it to work and receive the grateful thanks of the parents.
But it didn’t work.
We checked the blood sugar again, and it had come back up to normal levels, yet the condition of the girl was unchanged.
So we (rather quickly) took her into hospital – we haven’t been back there yet to find out what had caused her confusion. Was it drugs, alcohol, psychiatric problems, CVA (cerebrovascular accident) or even just a bad nightmare? Once we get back to the hospital which we took her to we will no doubt be able to find out. She didn’t have a high temperature, didn’t have any medical history besides the diabetes, her pupils were normal and responsive; all observations were normal.
We spend a lot of time dealing with things that are simple to cope with. You can fix them almost by rote thinking, but every so often you get a job that throws you off balance. Normally you ‘wake up’ and deal with it by going back to basics, but other jobs just completely confuse you, and this was one of those jobs.
This post got me a large number of people coming to my site looking for the search term ‘Daddy fucking daughter’. Sometimes the Internet is a scary place. It turned out that the girl had been drinking vodka, and that this was the reason behind her confused and combative state.
ORCON!
ORCON – the biggest problem with the ambulance service, and the biggest cause of staff/management friction. Every so often I will revisit this topic, as it’s of such importance.
I’m single at work at the moment (which means I don’t have anyone to work with – so am sitting on station twiddling my thumbs), so I thought I’d tell you all about the great God ORCON and how he rules the life of every EMT/paramedic in England.
This is really boring, so I’ll not be hurt if you don’t bother reading any further.
The government likes to give everything targets, from school grades, the waiting time for breast cancer referrals to the number of trains on time.
The ambulance service has only one main target to reach, that of ORCON. ORCON was started in 1974 and governs how fast we are expected to respond to ‘Cat A’ calls. (‘Cat A’ calls are our high-priority calls, although because of the way calls are assessed, they are rarely seriously ill patients).
Essentially, for every ‘Cat A’ call in London we have to be there within 8 minutes.
Simple really.
It doesn’t matter what actually happens to the patient, just so long as we get there within 8 minutes. For example, if we get to someone who has been dead for 2 days within 8 minutes, that counts as a Success. If we get to a heart attack in 9 minutes, provide life-saving treatment and ensure that their quality of life is a good as possible it counts as a Failure.
For those who don’t live in London, let’s just say that traffic is often heavy, and there are speed-bumps and tiny side-roads. We have more than 300 languages spoken in London, which may delay getting the location we are needed at. We are hideously overused and understaffed, we face delays at hospital owing to overcrowding and delays on-scene because of the ignorant people we have to attend to.
None of this matters – all that matters is the 8-minute deadline. If we make 75% of all calls in 8 minutes we get more money from the government, which means more staff, vehicles that work etc. … If we don’t make 75% then we don’t get any more money and we continue to struggle. This year it looks like we are going to make it, but only just.
There isn’t any reason behind 8 minutes being the time we need to get to people: brain death occurs after 4 minutes or so; trauma, while needing to be treated as quickly as possible, has the ‘Golden Hour’. The current rumour is that it is how long MPs have to vote when the Division Bell rings in parliament – who knows? No-one I have spoken to has any decent answers.
Well, that should be the last of my posts on the boring ‘day to day’ running of the London Ambulance Service.
You may all rejoice now.
Oh … Bollocks …
Rather obviously this topic dominated my weblog for some time – I’m including only some of it here, because I’m sure that you didn’t want to pay good money to read about me being horribly ill. I haven’t edited this post for this book – it’s much how it originally appeared on my website. I started writing it less than 2 hours after I was exposed.
There is a fear that every health-care worker has. Tonight that fear jumped up and slapped me in the face.
Second job of the shift, we were called to ‘50-year-old male – collapsed in street’. Normally this is someone who is drunk, but we rushed to the scene anyway, just in case it isn’t (we rush to everything – it’s the only way to be sure you are not caught out). We reach the scene and see the male laying on the floor talking gibberish. He is bleeding from a cut on his face and possibly from his jaw. Bystanders tell us that he ‘just dropped’. He then starts to vomit, and because it’s dark we get him on our trolley and into the back of the ambulance.
Our basic assessment finds that he has no muscular tone on his right side, although all his observations are within normal limits. Deciding against hanging around we start transport to hospital. Halfway to hospital he starts to vomit and cough – part of this vomitus/blood flies unerringly across the width of the ambulance …
… right into my open mouth.
Pretty disgusting, but what can you do? The patient then starts to come around, now able to move all limbs and to talk. This is good, it means I’m able to get some history from him. So I get his name, date of birth, address. Then I ask this 50-year-old if he is normally fit and well.
‘No’, he says, ‘I have AIDS (acquired immune-deficiency syndrome)’.
Bollocks.
I’ve never had anything from a patient in my mouth before (apart from the odd chocolate when I was a nurse), so of course the first time is with an HIV (human immunodeficiency virus)-positive patient.
My crewmate looks in the rear view mirror, and that look passes between us. Ambulance people will know what I mean – it’s the ‘Oh shit’ look that you give/get when something goes horribly wrong.
We get to the hospital and the patient is looking a lot better, fully orientated, full strength and starting to feel the pain from a probably busted jaw. So I get to hand over to the nurse, which turned into a bit of a comedy moment …
Me: ‘Patient witnessed collapse, had right-sided hemiparesis, now resolved. Previous history includes AIDS’.
Handover Nurse: ‘Fine’
Charge Nurse: ‘You can’t say that’
Me: ‘Pardon?’
Charge Nurse: ‘You can’t say AIDS – people will be prejudiced against him’
Me: ‘Well they shouldn’t be, and this is medical stuff. It’s a syndrome like any other’
Charge Nurse: ‘You have to call it something else’
Me: ‘I don’t really care for political correctness, besides I’m a patient as well – I swallowed some of his blood’
Charge Nurse: ‘Oh, well … lets get you sorted out then’
I then went through the rigmarole of having blood taken, then I asked to be put on PEP, which the charge nurse agreed I should be put on. PEP is ‘Post Exposure Prophylaxis’ – basically a cocktail of antiretroviral drugs that, taken over a 4-week period, will hopefully reduce any live virus to non-infective amounts. Common side-effects include nausea, vomiting, headache, diarrhoea, cough, abdominal pain/cramps, muscle pain, tiredness, flu-like symptoms, difficulty in sleeping, rash and (I love this one) flatulence.
Other more uncommon side-effects are … pancreatitis, anaemia, neutropenia, peripheral neuropathy, and other ‘metabolic effects’.
I’m in for a barrel of laughs for these next 4 weeks …
The charge nurse looked really sympathetic when he offered me stuff to look after the side-effects – he used to work in an HIV clinic so I guess he knows better than me what I’m in for …
Then we talked about rates of infection, which is why I’m feeling kinda relaxed here. HIV is a tough virus to catch (compared with hepatitis, which is the one that worries me). If I were to stab myself with a needle after drawing HIV-positive blood I would have a 0.004% chance of catching the virus. Swallowing a bit of blood/vomitus is less risky than that, especially as I have no mouth/stomach ulcers. With the PEP my chances of ‘seroconverting’ are as close to zero as you can get. I knew all this before I set foot in the hospital, which probably explained why I wasn’t a quivering wreck.
So far ‘only’ two medical workers have seroconverted after needle-stick injuries. I greatly doubt that I’ll be the third.
So ‘The Plan’ is that I go to see Occupational Health on Monday, and they will advise me on what happens next. I’ve been told already that I’ll have to avoid sexual contact for the next 3 months (not a hardship – I’ve managed ‘no sexual contact’ for 2 years before now) and that I’ll probably need to take 4 weeks off work due to me feeling too ill from the side-effects of the antiretrovirals.
We’ll see about that … I don’t ‘do’ ill.
Anyway, if I do need to take time off it’ll give me a chance to read some books I’ve got sitting on my shelf – and complete ‘Zelda – Windwaker’.
Gotta go now, I feel flatulent already …
I never got around to completing ‘Zelda’.
‘Donor’ Takes on New Meaning
I got a lot of support over the previous post, and to be honest I would have been a lot less calm if I didn’t have my blog where I could offload some of my worries.
First, thanks to everyone who has contacted me over my ‘exposure’, I appreciate it all, even if I haven’t personally replied to you (you’ll find out why I might not have answered you a bit later in this post …).
I went to Occupational Health on Monday, basically to let them know about my exposure, and that I was on PEP. The LAS showed how nice they are by lending me a spare ambulance to drive to my appointment – GPS navigation comes in handy when you don’t know where you are going.
Occupational Health is south of the river at King’s College Hospital, which is a bit of a trek. ‘Occy Health’ took baseline blood samples, so they would know if there was any effect on my liver/kidneys/white cell count, and filled in a couple of forms about my exposure. Then they told me that they would get in contact with the ‘donor’ to see what his virus load and hepatitis status was.
Until now I always thought of ‘donor’ as a ‘nice’ word – heart donors and the like – I never really thought it would happen to include this circumstance.
During the consultation they told me that I’d need blood tests every fortnight for the next month and a half, and that my first HIV/hepatitis status check would be in 3 months, with an additional one in 6 months. Should they both be negative then I would be in the clear.
They also told me of the side-effects of the antiretrovirals that I am taking, and seemed surprised that all I was experiencing was similar to a mild hangover.
That was yesterday – today was spent vomiting/sleeping to avoid nausea/and experiencing the joys of explosive diarrhoea.
My station officer called up and asked me how I was. When I told him, he basically told me to take it easy and go back to work when I felt better.
However, there was some good news when the Occupational Health nurse contacted me, and told me that the donor’s viral load was low, that there were no resistances to the PEP drugs I’m taking and that in 2002 he was free of hepatitis. That has eased my mind somewhat.
Some people have commented that I’m taking it rather well. There are a number of reasons for this, not least that the chances of me becoming HIV-positive are less than 1 in 5 000. The other thing is that I can’t do anything now to change those odds, apart from continue to take the PEP.
The other side-effect of the meds I’m taking are that I’m having a certain ‘vagueness’: my mind isn’t operating on all four cylinders, so if this seems disjointed, I’ve got an excuse …
Even today I’m not sure that the PEP drugs didn’t permanently ‘disjoint my mind’.
Pavlov’s Dog
Well, the PEP is still going down, unfortunately I’ve developed a Pavlovian response to the hours of 8 o’clock. Every 12 hours I need to take the pills – I start to get nauseous just thinking about it, the familiar copper taste hits my mouth and I just want to lie down.
I also seem to have lost any control over my circadian rhythms, I’m sleeping for 14–16 hours straight and I’m drowsy for the rest – doesn’t matter whether it is day or night.
At the moment the rather wonderful ‘Scissor Sisters’ album is chilling me out nicely, particularly ‘Return to Oz’ (which has a bit that puts me in mind of The Kinks’ ‘Lola’).
I am, however, losing the motivation for cooking food, not least because of the large amount of washing up accruing in my sink. It makes me feel like a student again.
Also, my PC is screaming out for a complete overhaul – I just can’t be bothered.
Mothering Sunday
Well, Saturday was the last day I worked but Greenfairy (another blogger) mentioned something that I wanted to write about – but forgot, for some bizarre reason …
The first call of Saturday was to a ‘?Suspended’.
(#litres_trial_promo)
So we hack along the road, knowing full well that because it is the first job of the day the patient is definitely going to be dead.
We arrive at the house and the FRU is there before us – I grab my kit and bound up the stairs past the daughter who called us and into the bedroom. Where a very dead lady was lying on the bed while the Rapid Responder was completing his paperwork.
One look is all you need to tell if someone has been dead for some time – and this lady had that look. It turned out that the daughter last saw her mother alive an hour ago, but that she was feeling a little unwell and took to bed. The daughter had checked on her half an hour later and found her not breathing. She then waited 20 minutes to call us as she was in such a ‘tizzy’. A quick look told us that even if we had been there when it had happened it was unlikely we could do much: various clues led us to think that a stomach ulcer had ruptured and she had bled out into her stomach.
All around the house were flowers and cards – the next day being Mothering Sunday.
No sooner than we had informed the daughter that her mother had died than the doorbell went and my crewmate went down to see who it was. It was only a bleedin’ flower delivery man, delivering flowers to the (now) dearly departed. My crewmate told the delivery guy that now, perhaps, wasn’t the best time to bring flowers but took them in anyway, hiding them in the kitchen.
Perfect!
Then we had to wait an hour for the police to turn up, which is normal procedure for any death in the home and is nothing to worry about. I then helped the police turn her body (to look for anything strange) and put my hand in a puddle of urine
(#litres_trial_promo) – something that wouldn’t bother me, IF I was wearing any gloves.
Oh well.
The Other Guy
I’m feeling a little better, the side-effects of the PEP seem to have subsided somewhat, although the flatulence is reaching epic proportions, which, coupled with the diarrhoea, makes every bowel motion an adventure
I have my second date with Occupational Health on Friday, for a blood test to make sure that the PEP isn’t battering my liver/kidneys/pancreas and that my white cell count hasn’t lowered. Work have said they’ll do everything they can to supply a vehicle to get me down to south-east London.
I’ve been thinking a bit about the ‘donor’; I wonder how he feels – he’s lying in bed after having a rather frightening collapse in the street, with a broken jaw and the reason for the collapse unknown. Then a couple of days later the medical team ask him to consent to some more blood tests because he may have infected the EMT who helped him out.
If it were me I’d be absolutely mortified.
When I talk to Occupational Health I’ll ask them if they can get a message back to him, letting him know that I’m fine and that I don’t blame him for anything. I know his name and address, but I don’t think it’d be right to turn up on his doorstep to talk to him.
I hope he is alright and that the collapse was something simple – I suspect a ‘TIA’ (transient ischaemic attack), which can be a precursor to a stroke, but with the right medications hopefully the threat of that can be controlled.
I never got to see him again, so he never found out the results of my blood tests. I kind of hope that he gets to read this, so he knows that I’m fine.
Twelve Hours to Go
In 12 hours I will have stopped PEP. Those seven pills are the last ones that I am going to take.
I am extremely happy about this.
It has been a month since my stomach didn’t feel as if I were waiting to vomit, a month since my thought processes have seemed even remotely like mine. A month since I last worked – good grief, am I bored! A month of wondering if my life is about to change for the worst. A month of my mates looking sideways at me when I had to take the pills in front of them (but still friends enough to laugh and joke with me about it). A month of having to get out of bed to eat breakfast, because the pills need food in my stomach. A month without shaving (why bother, I’m not allowed to have sex!). A month of feeling just the tiniest bit isolated. A month of people who I have never met, from places around the globe I have never seen, wishing me well. A month of always feeling grateful to those people, for this is the kindness of strangers – in itself a random act of reality.
All over now.
In two months I get to go for my HIV test, which should be fun and giggles.
But for now – I’m happy.
I really think that if it wasn’t for my blogging and the support of my friends around the globe I’d have gone mad from boredom. My next book should be Blogging as a Mental Health Exercise.
Proper Day
My first ‘proper’ day back at work, working with my new crewmate on a proper ambulance.
The first job was a 66-year-old male who had been fixing tiles on his shed roof and had fallen off the ladder, probably around 10 feet. He was shut behind his front door and all I could hear through his letterbox was ‘I’ve broken my leg’.
The police are much better than me at getting into locked premises (the last time I tried I fell on my arse in front of a crowd of 20 people) so we waited for them to arrive and use their specialised equipment (screwdriver/size 12 boot) to force open the door.
Gaining access to our customer it was pretty obvious that he had fractured his femur (thighbone) as it had a new bendy section just above the knee. The pulse was good in his foot and he didn’t complain of pain anywhere else in his body. This brave man had crawled, with this fracture, from his garden through his kitchen to the living room where he kept his phone. All throughout our treatment he didn’t complain once. We splinted his leg and ‘collared and boarded’ him from the house (a fall of 10 feet can easily break your neck, and the pain from his leg could easily distract him from a neck injury). We could have set traction on his leg, but we were only 5 minutes from the hospital; so we ‘blued’ him into Newham General Hospital, where he was ‘attacked’ by the local trauma team.
The next job we got was a dinner lady at a local primary school who had dropped a knife on her foot. There was a tiny cut to the foot, and after cleaning, dressing and checking her tetanus status we left her at work. What depressed us was that there were no scraps of food left we could have.
Driving back from the last job we saw four workmen chasing another man who ducked into the local mosque. We ignored this until we got a call to the area the men had run from – apparently a man had been assaulted with a ‘Car-lock’. HEMS (our emergency helicopter service) had been activated and were going to make their way to the scene. When we did a quick U-turn and rolled up to the scene it soon became obvious that HEMS was not needed so we cancelled them. The man had been clamping an illegally parked car when the owner and his wife returned. The car owner then pulled a large aerosol can from his boot and hit our patient around the back of the neck, causing a short period of unconsciousness. His wife had also put up a fight, but the owner of the car had run (into the aforementioned mosque) leaving his wife behind. (What a gent!) At one point we thought it was going to turn into a riot as 30 youths from the mosque were adamant that the four workmen doing the chasing weren’t going to set foot in the mosque.
Again, we had to collar and board him, and lift him onto our stretcher, which wasn’t much fun as the man weighed at least 20 stone. Subsequent treatment at hospital showed no serious injuries.
Final job (after having to get our nice, new, shiny ambulance fixed – a problem with the side-door) was a 60-year-old female collapsed at a bus station with slurred speech and ‘not drunk’. Remember that, ‘not drunk’, it’s important.
What could it be? Could it be a stroke? Could it be hypoglycaemia? Could it be cardiac related? So we turned up to find ‘Mary’ having fallen over, smelling strongly of alcohol and with a 5/6ths empty bottle of whisky in her purse. (My crewmate had to tell me about the smell of alcohol, as I’ve mentioned before, I’m pretty much unable to smell it myself.)
‘Not drunk’ – why did the callmaker say that? It’s bloody obvious she was pissed as a fart. I’d guess it was the bus station staff who wanted her gone and were afraid we wouldn’t turn up if we knew she was drunk. Still, it was an easy last job of the shift, even if she did keep grabbing at my balls and kissing my (thankfully) gloved hand.
This counts as a good day.
Now I’m off for some endorphin-releasing Bailey’s ice-cream.
Can you tell I was deliriously happy to be back at work?
These Boots …
These Boots …
Have walked along train tracks
Have been washed in the blood of murder victims
Have kicked in doors to get to unconscious women
Have stepped in more urine, in more tower blocks, than I’d care to think about
Have kept my feet warm and comfortable on long nights
Have been allowed into a mosque
Have climbed fences to reach dead bodies
Have run across football fields to try to save a life, and failed
Have been spat on, vomited on and shat on
Have stood in ‘remains’
Have tried to find purchase while walking backward down narrow stairs
Have defended me from drunks and druggies
Have been run over by a 22-stone trolley
Have been stared at by a daughter when I was telling her her mother had died
For Pixeldiva who denies she has a shoe fetish.
Gamma GT
I went to Occupational Health today – it seems that the last time they checked my blood (because of being on PEP) my liver enzymes were a bit elevated. Most significantly my gamma-GT (gamma-glutamyl transpeptidase) was at 164 (it should be between 0 and 55). PEP is well known as having effects on the liver, so this isn’t completely unexpected.
More blood was taken today to check that the enzymes have returned to normal. The nurse was very concerned that I was alright in having my blood drawn, and that I wouldn’t faint. She was asking me this while I’m sitting opposite her in full uniform …
The nurse was also a bit surprised that I’d had aural hallucinations and looked at me as if she thought I was turning schizophrenic – I assured her that the ‘voices’ were now leaving me alone and that it wasn’t a problem. She’d never heard of this symptom before, so at least I entertained someone today.
Deaf Old Women
Nobby is working tonight from our main station. He is always a good laugh and always seems to have a joke whenever he works. Tonight I met him outside the hospital and he told me about a deaf old woman he had just brought in.
It was raining as he started to wheel her out her house so he made the comment ‘It’s raining, you picked a fine time to be ill’.
‘Eh?’ was the reply.
‘The rain … it mucks up my hair’.
‘Eh?’
‘MY HAIR!’
With this she took a long hard look at Nobby’s very short, and very receding hair and asked him, ‘Is it because of cancer?’
It is now 3 a.m. and already every other patient we have picked up has been drinking – from the 38-year-old male having a panic attack, who didn’t want to talk to us, to the 50-year-old female who slipped on some steps coming out from the pub and cut her head. This has so far ended with our last call being one of our smelly ‘frequent flyers’, who thankfully decided not to hang around and wait for us to turn up.
Then there was the police car that managed to accidentally force another car into someone’s garden – one of those jobs where every passing car slows down to stare. Thankfully, there were no injuries, apart from the house-owner’s disturbed sleep. (At least I assume it was the owner – he was dressed in no shoes and a dressing gown.)
With a bit of luck people are now wrapped up nice and snug in bed – away from the rain – and the only calls we will get will be the 5 a.m. ‘I’m in labour’ call that will result in a baby around 11 a.m. (long after I’m in bed).
Hand Over Mouth
No sooner do I hope for a quiet hour or two than the activation phone goes; it’s sending us 200 yards up the road to a ‘Collapsed Male’. We are met by two police officers who tell us that the patient was walking along the street, saw the policemen and then collapsed.
We get to the patient and my crewmate can’t smell any alcohol on him, but he is coughing and spluttering like an Oscar winner. He complains of a headache, coughing, leg pain, back pain and an inability to walk. Other than that he is refusing to talk to us. Examination is normal and the patient is obviously play-acting.
He then does one of the things that I really hate (given the prevalence of tuberculosis in Newham); he coughs all over us and the vehicle without putting his hand over his mouth. Then he starts to spit on the floor of the ambulance, again something I take a dim view of – but I’m driving so I leave it to my crewmate to sort out.
Forty seconds later and we pull up outside the hospital, and our patient decides to roll around the floor. By now our patience is wearing thin, so we haul him up and throw him in a wheelchair.
In the hospital he refuses to speak to the nurses, says he cannot stand and doesn’t acknowledge any requests. We leave him there and within 30 seconds are back on station.
While at the hospital I indulged in a little bit of teaching. The nurse who was assessing our patient was trying to check his pupil response (by shining a light in each eye and making sure that it reacts to light) but the eyes don’t appear to be reacting. I then suggest turning off the ceiling light that the patient is lying on his back staring at.
I still have patients who insist on coughing without putting their hand over their mouth. I’ve given up asking them to stop – instead I just give them oxygen, via a nice tightly fitting oxygen mask. I got a lot of people coming to this post searching for ‘Hand over mouth’. I swear I don’t know why.
Essential, Not Emergency
One of the bizarre things about the Ambulance Service is that, in the eyes of the government, we are an ‘essential’ service but not an ‘emergency’ service. We are ‘essential’ because the emergency services (Police, Fire Brigade and Coastguard) are run by the Home Office but Ambulance Services across the country are run by NHS Trusts, and as such do not have access to the same resources as the true ‘emergency’ services. The distinction is often slight, but can sometimes have quite important considerations for our safety.
Last night was a case in point. We were called to a patient with abdominal pain; however, further information was given that the patient could be violent. There was something in this information that triggered my ‘danger-sense’, so I was happy to wait for police assistance to arrive before approaching the house.
Four police officers turned up – normally only two are sent to assist us – and they told us that their computer system, and their personal experience with the householder, showed him as a nasty piece of work. We followed the police to the patient and they told him that they were going to search him, and that they wanted to put him in handcuffs first. The patient had obviously been involved with the police before, as once he was handcuffed they checked to see if he had any new warrants out for his arrest …
Searching him they found a large stick, and a rather worrying-looking (5-inch) knife on his person.
All through this the ‘lady’ of the house was shouting abuse, mainly at the patient, but occasionally at the police officers present. One quick examination showed nothing life-threatening, so we offered a trip to hospital, which the patient accepted. However, as we left the house the woman shouted a few final obscenities at the patient and he then told us he couldn’t be bothered to go to hospital and stalked off into the night. (This was not a problem for either my crewmate or myself.)
Police computers had information that he was dangerous (a number of rather vicious assaults) but our computers are not allowed to have such data. A police dispatcher has told us that they have all sorts of information on addresses, from animal liberation protesters to Members of Parliament. Again, our computers don’t have any information of that sort unless we enter it manually after an ambulance crew has been threatened assaulted.
Needless to say, one such report has been sent to central office.
I later found out that the patient was addicted to crack cocaine – which explains a lot.
Return of Pavlov’s EMT
Last night we picked up an alcoholic who is HIV positive. I (still) have no real fear of HIV patients, even when they are bleeding a bit and this patient was not (although they had wet themselves). The only problem is that I seem to have turned into one of Pavlov’s dogs. When we found out the patient was HIV positive my stomach churned as if I were back on the PEP. It was really rather strange because it wasn’t fear (I’ll only have that when I’m due for my HIV test) but instead something more … biological.
The son of the patient was extremely embarrassed at the antics of his parent, and my crewmate spent some time making sure that he was alright.
Naughty?
Is it naughty to take someone to hospital, who doesn’t really need to go, just in order to get a fry-up breakfast there?
It’s a lot simpler to take everyone to hospital whether they need it or not. It means that I have to do less paperwork, the patient feels validated and it means that if I’m missing something nasty (which is likely to happen at 6 a.m.) then the hospital has a chance to catch it.
Too Darn Busy
I am extremely busy at the moment; I’m often posting from my PDA (Personal Digital Assistant) and mobile phone. I should be catching up with stuff on Friday (including answering all those comments people have left).
Got some blood results (post PEP stuff), seems my white cell count is still going down. I think they have a life-span of 120 days, so it might get lower before it gets better. Still, it gives me an excuse to see the rather pretty occupational health nurse.
Today we did the usual of little old ladies who feel unwell calling their GP and the GP calling us to take them to hospital because they are too busy to drag their arses out of their office to visit sick people. On the radio it seems that lots of people are dropping dead – the weather is quite a bit warmer (24°C) so the old are placed under a bit more physiological stress.
I have a 101 things to do, and no time to do it – simple stuff like paying bills can be incredibly hard when you are single and a shift worker.
And I think I’m moaning too much …
I’m off to bed now. Goodnight all.
How Not to Stop a Stolen Car
So damn tired …
I’m currently at that point where I wonder whether I am hungry enough to cook dinner before I go to sleep. Which biological urge will win out?
Today, our Control wanted us to go to an emergency call when we were the other side of the Thames – I rather politely asked them if we were the nearest motor as we weren’t actually a boat, the reply was, ‘Yes, do you have your water wings?’ So we ended up going a couple of miles out of our way to cross the river.
The call was a faint, probably from the heat that is roasting London at the moment – at least the women are wearing revealing clothes, which makes our job of cruising through the streets a bit more enjoyable.
Picked up two psychiatric drug-using patients in a row who were drunk and lying in the road perhaps 500 yards away from each other. Some children were poking one with a stick …
Then there was the 51-year-old 4-foot-4 Asian grandmother who, upon seeing her husband’s car being stolen, jumped on the back and hung onto the rear windscreen wiper. She was flung off and, thankfully, not seriously hurt – mainly bruising and gravel rash. Unfortunately, the car that was stolen also contained her house keys and bank books. The A&E was so busy they had to put her out in the waiting room – something that annoyed me no end, especially as the nurse that put her out there had annoyed me earlier in the day by suggesting that I didn’t know what the symptoms of bulimia were.
Now to eat/sleep … then lather/rinse/repeat tomorrow.
Sunday
Sunday alone in my flat, no work, no stress, some decent stuff on telly = Good.
No chocolate in the fridge, uniform to be ironed, work tomorrow = Bad.
Phone call from Occupational Health telling me my blood values are back to normal = Excellent (only HIV/hep test to go now).
Eight … Nine Down
Our complex is EIGHT ambulances short today, so it comes as no surprise that we are running around like the proverbial blue-arsed fly. Control keeps broadcasting jobs for which they have no ambulances, this means that a lot of crews are more unhappy than usual, as Control hassles us about ‘greening up’ quicker. It doesn’t bother me, if I’m busy doing jobs it makes the shift go quicker.
As I’m typing this an ambulance has had a blow-out on the fast lane of the A102 – a very busy road. The crew are alright, but it means we are now nine ambulances down for the next 2 hours at least.
The jobs I’ve been doing are the usual Monday morning sort of stuff: 97-year-old women having heart attacks, 10-year-old boys with cut heads (a rather impressive 3-inch cut, mind you) and 88-year-old men from nursing homes who have ‘high blood pressure’ (they invariably have a better blood pressure than I do).
Now some silly sod has stabbed himself in the stomach with a pair of scissors.
Health Copyright
I’ve been on a ‘Guidelines’ course. Essentially, this is a course that tells us that we are already doing the right thing; it also introduces us to a book with our new treatment guidelines. It takes 2 days and tomorrow will include learning about child abuse (do we have to bring our own child?). So far the course has been a trainer telling us that this course changes nothing, and we are to continue doing what we are doing at the moment. At least the days are short, 8 a.m. until 2 p.m. At the start of every Powerpoint presentation is the same definition of ‘Clinical Governance’.
We had to write our own scenarios then swapped them around to other groups (this is a really easy teaching technique, since you don’t have to plan anything). There was also a chat about how our complaints to compliments ratio is about 50/50, and that most of the complaints are because of ‘staff attitude’. So far I have had no complaints, and no compliments – I’m a strong believer of flying under the radar.
However there is a problem – the Guidelines book we should be getting is version 3.0, but the book we are actually getting is version 2.2.
The reason for this?
Copyright!
It seems that the LAS wants to change a few bits to make it more relevant to London. But because the organisation that wrote it maintains the copyright it can’t be changed for us. Lawrence Lessig’s Free Culture states that you get value added when others can build on your work. This is a perfect example of this principle.
So, the people of London are not getting the best clinical care because of copyright.
Clinical Governance is about getting the best care to the public, so it’s a bit of a mixed message.
Venus Transit
There is a Transit of Venus today – all these special astronomical phenomena remind me of the eclipse we had in the summer of 1999 …
(Cue wobbly flashback video effects)
I was working in A&E at the time of the eclipse and thought that there would be no way I’d get to see it. Like all A&E departments this place had no windows and could be perhaps best described as a bunker. Today, however, the department was empty for the first time in living memory. Normally by that time of the day we would be packed full, but today … not a soul. One person had been in earlier with a painful foot, but there wasn’t the normal ‘trolleys in the corridor’ effect that was normal for that time of day.
We learned that day that CT (computed tomography) films make excellent sunglasses.
So, the whole department stood outside on the grass staring at the sun slowly disappearing – very spooky, and one of the few strong memories I have from that long ago. I suspect that many of the wards were empty as well: there was a procession of people wearing dressing gowns and holding tight to their drip stands wandering around the hospital grounds.
As soon as the eclipse finished we immediately had two cardiac arrests brought in by ambulance, it was as if they had waited until after the eclipse before deciding to keel over dead …
Life also tends to be a bit quiet around FA cup finals, royal marriages and important soap storylines.
Not All Bad
I often carry a camera around with me. I was talking to some kids recently – they were happy little buggers, enjoying the sunshine on a lazy Sunday.
It’s not all bad this job.
This picture still makes me smile.
Wedding Saga + Pub Fight
Some calls are a pain in the arse, not because anyone is particularly ill, but instead because you can see complaints coming in, and there being a high possibility of losing your job.
Tonight was a case in point. We got called to a wedding reception where the bride had collapsed; a quick history revealed MS (multiple sclerosis), and that it was likely that this was the cause of the collapse. Unfortunately, the patient and the patient’s new husband were adamant that she wasn’t going to go to hospital, particularly the hospital that was nearest. Things were not helped because they had called an ambulance for an aunt who had collapsed, but had cancelled it before it had arrived because it was ‘taking too long’.
While we were getting a history from the patient, the new husband was generally acting like an arse: he was questioning everything that we did, interfering with our talking to the patient and generally getting in the way. We managed to get rid of him for a short period and the rest of the family came over to us and apologised for his behaviour.
Luckily, the patient’s hotel was next door to the hospital so, after 45 minutes of persuasion, I managed to get the patient to agree for us to take her towards the hotel, and if she felt better then we could, in good conscience, leave her there. En route I called up on the radio, and arranged for the Duty Officer to meet us at the hotel. He did and the responsibility of leaving her without treatment now fell on his shoulders (thus, saving our jobs should anything go horribly wrong).
I know MS is a horrible disease. I know it isn’t fair that it would strike on your wedding day, and I can understand why you might not want to go to hospital … but if you can’t move half of your body, then please understand why the ambulance people might be a bit unhappy to leave you lying in the middle of the street.
It then all kicked off in the Hackney/Homerton area. There was a big fight in a pub, with everything in it being smashed – multiple casualties with various head and facial injuries from flying bottles and broken glass. We were first on scene, and I needed to call up to let Control know that at least another 3 ambulances were needed. At least it gave me a chance to practise my ‘5-second triage’ skills. None of the drunks there were particularly aggressive, but there was a ton of police there pulling me from one casualty to another around the pub, and even 300 yards up the street. This was just a taste of what was to come as another pub was attacked and it basically overloaded our resources. It got so busy that our Duty Officer was transporting severe asthmatic attacks in his car (and he doesn’t carry much more than a defibrillator and oxygen) and Control was holding 35 calls across the area. That is, 35 calls at 3 o’clock in the morning. That’ll teach me to wonder if it will be busy in a previous post.
Tomorrow England play their first ‘Euro 2004’ match – Alcohol + Patriotism + Recent History (we are playing the French) + Me Working = Recipe for Disaster
Watch this space …
I never got a complaint from that job, although for some time I was holding my breath about it.
Kick Off
Well it looks like I was right, the nice weather with people in the pubs from an early hour, coupled with England losing 2–1 in the football, has led to what can, in best tabloid fashion, be described as ‘an orgy of violence’.
It started out with a couple of ‘glassings’, which we have been getting over our vehicle computer screens as ‘stabbing to the head’ for some reason.
A couple more assaults, including one who was set upon by a number of drunks who were intent on stealing his car. Luckily he was not too badly injured – more shook up. Other crews were ‘blueing’ in a number of assaults, including at least one stab victim.
The police were running from call to call, and once more there are not enough ambulances to deal with the large number of calls we have been receiving. Our Duty Officer has been telling crews that we should be wearing our stab-vests constantly – but he isn’t the one who has to lug a 20-stone unconscious patient down 4 flights of stairs in this heat …
Good job I’m not searching for a quiet life.
I am, however, off to bed now.
Only One Stabbing
For the first night in ages it has been reasonably quiet on the streets of East London – only one stabbing and that was to the patient’s arse …
However, while adults are no doubt nursing hangovers the children are out causing mischief. The first two calls we got yesterday were to kids (8 and 10 years old) who had been hit by cars. The first was a ‘classic’: child running out towards an ice-cream van. He was alright apart from a broken right ankle. No sooner than he was safely ensconced in hospital than we find ourselves dealing with a child who has run out in front of a car (in the absence of an ice-cream van) and has broken his left ankle.
Tie in a hyperventilating adult, a 14-year-old with hay-fever and a drunken Colles’ fracture and you have a pretty good night.
We had one serious job, someone who had a CVA (a CVA is a ‘stroke’) on a train. The CVA wasn’t so much the problem as the extrication of the patient, who couldn’t move, and yet was combative with his unaffected side. To start off, the space between the seats on the train was not large enough to allow our carry-chair to pass. The man was large and heavy so we basically had to manhandle him (in a very undignified manner) through some connecting doors and out onto the platform. The train station has a big flight of stairs towards street-level and only one lift, and the lift was not on the platform we were on. It would have been unsafe to carry this man up the stairs because of his weight and combativeness. In a rare spark of genius I realised that if we waited for a district line train we could carry him through the train onto the other platform. We ‘blued’ him into hospital as his pulse-rate was 40 (should be 60–100).
When I went to see the patient later in hospital he had started to regain his speech and wasn’t confused. He was about to go for a CT scan so, with a bit of luck, he might make a good recovery …
This is just another part of the job that I like – that sometimes I have to out-think problems. I can’t see me doing this in an office job.
Good Shots
There is something that I’ve learned over many years of health-care work. When you are lifting little old ladies with senile dementia, they will sometimes grab you by the testicles.
And squeeze …
This hurts.
I swear, the greater the degree of dementia, the greater the accuracy and the stronger the grip.
And for the love of all that is holy …
Don’t drop them.
That hurts even more …
Ethnic Dress
When I went to the Clap Clinic for my HIV test, I was referred to a ‘Health Adviser’, which is a new name for Counsellor. I am, as regular readers may appreciate, a fairly simple, pragmatic person: within hours of my HIV exposure I was aware of transmission rates, odds of infection and the rates of death caused by electrocution (1 in 5 000) and shooting in America (1 in 2 500). So, to be honest, counselling was the last thing I needed.
I did a counselling course when I was a nurse, and it did nothing to disabuse me of the notion that all counsellors are hippies who consider themselves ‘worthy’.
She asked me a load of questions about how I would cope if I were to be found HIV positive (answer: get over it), and cautioned me not to tell anyone I was testing, unless I was happy for them to know the result (answer: the whole world could know – if they read this site). There was some other stuff that is just too dull for words, and definitely too dull to read.
The thing that amused me the most, however, was not that the ‘Advice Room’ had the only comfy chairs in the place but that the counsellor was wearing a sari (the Indian dress). In and of itself not unusual, except that the woman wearing it was ‘whiter’ than me.
I’m well used to ‘white’ women wearing various Muslim dresses – it’s a religion after all – but as far as I’m aware a sari is a cultural thing. I’m guessing that in her ‘equal-opportunities, worthy, multicultural’ world that she is proving how non-racist she is. This is handy because to be honest out of the 20 or more people at the clinic I was in a race/culture minority of one. Not a problem, I know Newham well … it’s very diverse, but I wonder if Asian people would be impressed or nonplussed by her wearing a traditional Indian dress?
Maybe I should start wearing nothing but a Papuan penis sheath?
The HIV test result should be received by the 28th …
I’ve tried as hard as possible to make this sound as non-racist as possible – at no point have I meant to cause offence. I hate no ‘race’ more than another – I hate them all.
‘I hate them all’ – a philosophy to live by.
Small Victories
Our second call of the day was to an address where the elderly woman who lived there was believed deceased – the neighbours had called the police, and the police had called us. What this often turns into is us struggling to gain entry to the house, normally resulting in an injury to me, only to find someone who has been dead for some time.
We rolled up to the house and met with the neighbours who led us around to the back garden where, peering through the rear window, we could see the old woman sitting in her chair looking pale, still … and very dead.
Simultaneously, my crewmate and I jumped back in shock as we saw her take a breath!
She was breathing about six times a minute, and surely didn’t have much longer left to live – I rushed around the front and kicked in the front door (in one hit – something I’ve never managed before) and we got her out to the ambulance in double-time. We quickly decided that it would be wrong to ‘stay and play’, instead opting to ventilate her via ‘Ambubag’ and to monitor her cardiac rhythm and her pulse (which was strong and regular).
The hospital had a team standing by, as we had notified them of the patient on leaving the scene. The transport time to hospital was about 2 minutes, and on arrival the A&E team leaped into action, intubating and ventilating her, gaining venous access and running the various blood tests. Family members were contacted and plans for her treatment were drawn up. At no time did I feel that this 88-year-old woman was receiving anything other than the best treatment possible.
We cleaned the ambulance and restocked before going onto our next job; each time we returned to the hospital we popped our head into the Resus’ room to check how she was doing; there were plans to CT scan her head and to move her to ITU (intensive treatment unit). The family arrived and after some discussion it was decided that the best care for her was going to be palliative (that is to make her comfortable, but not to do any invasive procedures and to allow her to die). This was, I feel, the right course of action – the lack of oxygen would make any survival short and probably result in serious brain damage.
It has been a very long time since I’ve felt a great deal of sympathy towards someone, but this was one patient that I did actually care about, and not just because I’m soft on ‘little old ladies’. She had little chance of recovery, but we hoped for it anyway. She fought for her life, and had probably been doing that for the whole of the night. Because of our actions, and the actions of the hospital team, she wasn’t going to die alone, and she wasn’t going to die without her family saying a final goodbye to her.
It’s a small victory, but sometimes those are the only ones you get.
Right to ‘Load and Go’?
Yesterday we got a call to a 27-year-old male, diabetic having a fit. It was only 4–5 miles away, but travelling through Newham on a Saturday afternoon is always slow business – this was compounded by one of the roads which we use as a shortcut being closed for resurfacing. It took us 14 minutes to travel those 4 miles. Then it was up 5 flights of stairs into a flat where the first thing we could hear was hysterical sobbing. As I’ve mentioned before it’s one of those sounds you know means trouble.
Squeezing past a large bed we entered the bedroom to find a First Responder ‘bagging’ the young man, who was lying motionless on the floor. Sitting on the bed wailing, was a young woman who we discovered later to be his fiancée. The patient was connected to one of our cardiac monitors and it was showing sinus rhythm. Kneeling on the floor I did a quick pulse check – beat, beat, beat … then nothing, no pulse for 10 seconds. During the pulse check I was getting a history. Apparently the patient was an insulin-dependent diabetic, who had possibly been neglecting to take his insulin injections. He had become more agitated during the morning until he collapsed and started fitting after having an argument with his fiancée.
With a monitor showing an apparent sinus rhythm the patient was in ‘pulseless electrical activity’ – we can’t ‘shock’ this rhythm so I started CPR. From out of his mouth flew some bloody saliva, straight towards my face, luckily impacting on my forehead rather than ending up being swallowed (I don’t want to make that a habit).
One round of CPR (3 minutes later) and we got a pulse – the patient started ‘cramping up’, all his muscles had gone into spasm. A very quick blood sugar measurement reading showed ‘HI’ (a reading of over 32.0 mmols of sugar – the normal is 4–7 mmols). Immediately I started thinking of DKA (diabetic ketoacidosis) – a condition that occurs when blood sugar goes too high – a life-threatening condition that could explain his cardiac arrest. There was little that we could do on-scene as he needed immediate medical treatment beyond what we could provide.
With a ‘Load and Go’ order my crewmate set up the chair and the three of us dead-lifted him over the bed that was blocking the door and into the chair – I felt the familiar trickle of urine down my leg and looking at the patient he seemed to lose all colour. Another pulse check followed – his heart had stopped again.
I had to make a decision then: would we start CPR again only for him to continue this cycle of pulse/arrest, or do we make a run for the ambulance – all the time starving his brain of oxygenated blood – so that we could get him into hospital to correct the cause of his arrest?
I decided that we should ‘run for it’: if we got a pulse back it would be a purely temporary measure until his high blood sugar could be corrected. It was a very difficult removal – my back was spasming as we carried him down the 5 narrow, dark, winding flights of stairs and ran him across the 100 yards of pavement to our ambulance. Throwing him and his fiancée in the back of the ambulance we started the long run back to the nearest hospital. For 10 minutes I did CPR in the back of the ambulance while my crewmate tried his best to get through the exceptionally busy traffic – stopping and starting, swerving across the road, over pavements; he drove to the limit.
Throughout transport the only rhythm we had was ‘asystole’, which is when the heart isn’t beating at all. With our First Responder ‘bagging’ him and myself doing CPR we were doing all we could to support his life. During the transport the fiancée told us that he had had a previous arrest when he had stopped taking his insulin, but that he had, obviously, recovered.
Rolling up to the hospital we were met by the ‘Arrest Team’ – senior doctors from across the hospital. They descended on the patient, trying to get IV access, a secure airway and running diagnostic checks. It seemed, however, that the team leader didn’t want to listen to our handover. I was later told that he was concerned about getting the audit times right. The first thing he said was ‘the patient is biting on the airway’ suggesting that the patient wasn’t actually in cardiac arrest – because he hadn’t listened to my handover he didn’t know about the cramping episode earlier. The hospital staff did their own ‘pulse check’ and were confused about feeling a pulse (in a stressful situation doctors often feel their own pulse rather than the patient’s). It was only after some time that I could actually give the team leader a complete handover that he paid attention to.
The team worked on him for over an hour. His blood tests showed that his potassium was a sky-high 7.5; this was probably the main cause of his arrest. It transpired that the patient had renal failure and the high potassium and high blood sugar probably meant that the normal biochemical reactions in the body were being interfered with, leading to his fitting and cardiac arrest.
One hour later the patient was declared dead.
His fiancée was distraught; the patient’s parents had to travel 170 miles to the hospital and so it was necessary to tell them what had happened over the telephone – I can only imagine the drive down to London. The fiancée was convincing herself that it was her fault, that it was the argument that killed him, or that she should have recognised his symptoms of a high blood sugar before they became fatal. Both I and the nursing staff tried to console her, to tell her that it wasn’t her fault – but would the parents blame her?
I was thinking, would he have survived if we had remained on scene longer? Was making a run for it the right decision, given that I knew we had to carry him down the stairs? Would he now be alive if he had lived in a house rather than a flat? Did he die because he was an ‘angry young diabetic’ who didn’t want to comply with this treatment? He did have a history of taking an insulin overdose 2 weeks before.
It was a bad job, travel time was longer than it should have been, the flat was awkward to reach, it was difficult to remove the patient and the return journey to hospital was too long. It could have gone so much better. Although the patient might still have died it would have made us feel better. The job has left my crewmate and me a little depressed. Two deaths in as many days, one a ‘victory’, the other a real loss. I have today off so I’m going to relax and prepare for the joys of a night shift tomorrow.
One question for my medical readers: in the same situation would you ‘Stay and Play’, or would you ‘Load and Go’?
I got a couple of replies to the question above when I originally posted it online. The best was a mnemonic that I have taken to heart: L.A.T.E.R (Load And Treat En-Route). I don’t want to fool around on scene with a sick person who needs to be in hospital.
The Climax Draws Near …
I’m feeling a bit fragile at the moment – these nights are really taking it out of me for some reason. I think the main thing that is getting me down is that I should be getting my HIV test result on Friday; as predicted, I haven’t been worrying for the past 3 months (is it really that long ago?) but with the result due, it is sitting at the back of my mind nagging away. I’m confident that I’ll test negative – even so I have the framework for two blog posts, one Negative, and one Positive.
Either way, I think I’ll be having a drink or two after I get the result.
At the moment there is some confusion about how I actually get the result. The receptionist at the clinic didn’t know if their telephone text messaging trial was still being used – I suspect that on Friday I’ll hang around the ambulance station after the end of my last night shift and then walk down to the clinic and get them to give me the result at 9 o’clock. It would be cruel to make me wait until after the weekend …
… So it’ll probably happen, or they will have lost the sample or something similarly evil …
Tonight, the only job to really stick in my mind was a ‘purple plus’ (someone who has died and is beyond our help because of the amount of time they have been dead). It was an 85-year-old female who died, leaving behind her husband of nearly 70 years holding her hand. A very sad job, he was putting on a brave face, but I think later today it’ll sink in. Hopefully, his son will be with him when it does.
So, dear readers, the next update to this blog (unless my leg drops off) will be after I get my HIV result; I’m not in a frame of mind to write anything legible at the moment (as I’m sure you have noticed). Hopefully, my next post will be Friday, but I’m a strong believer in the inherent evil of the Universe … so I’ll talk to you on Monday.
Negative
Yep, the title says it all: the HIV test is negative, the syphilis test is negative and hepatitis tests are negative.
Needless to say I am so far beyond ‘relieved’ as to be numb with it all.
I spent the last 20 hours awake, first at work, then in the ‘Clap Clinic’ waiting room; I now think I deserve a deep relaxed sleep.
Goodnight, I’ll write more when I wake up …
Posted at 11:13 a.m. local time.
Fallout
Well … I’ve had some sleep so I can now post in a slightly more focused fashion.
First off, thanks again to everyone who has shown support, either through the comments box, or via personal emails – it’s all gratefully received. It looks like I’m going to have to find something else to die from now.
Tomorrow my brother and I shall be going for a nice relaxing drink, the first proper pub visit in over 3 months – there may well be a hangover involved.
I only had to wait 45 minutes at the ‘Clap Clinic’ for the test result – pretty hard to stay awake, but I think the emotional numbness that comes with exhaustion only helped me deal with the wait. The ‘consultation’ was over in less than 15 seconds: led into a room, asked to sit down and then told by a shaved-head counsellor that everything was fine. I didn’t have a massive flood of emotion (possibly owing to the aforementioned exhaustion), but afterwards I sat on a stone outside the hospital, rang my mum and brother, text messaged my old crewmate and breathed a sigh of relief. (Old crewmate told me that I had to go and repopulate Newham – something I don’t think I’ll be doing quite yet …)
Booze or Pot?
I didn’t sleep well last night – I think a total of an hour and a half – so if I’m a bit incoherent I’d like to register that as excuse number one. No real reason for the lack of sleep, it’s a disadvantage of rotating shifts that every so often your body clock just throws up its hands in despair and goes to sulk behind the sofa, leaving you suffering insomnia and/or intense fatigue.
Last night was actually quite pleasant. The first job of the shift (at around 4 p.m.) was given as an 80-year-old male collapsed in the street. Making our way there we were beaten by not only the police and fast response car, but also by a Duty Officer who had taken an interest in the job. It turned out to be a drunken Russian, actually in his early fifties, who had decided to lie down and sleep it off in an alley. I suspect he was very surprised when he woke up to find himself surrounded by three police officers and four ambulance bods of various ranks. He was a pleasant enough fellow, who didn’t speak a word of English, so to be on the safe side we loaded him onto the ambulance and took him to sunny Newham hospital. When we got there (and remember that this is around 5 p.m.) the crew before us, and the crew who followed us, both had people who were worse for wear for drink. Luckily for both our patient and the hospital a Russian nurse was working, so he could translate that the patient had indeed just drunk too much and would very much like to be left alone so he could go home. I’m always impressed by people who can speak another language, two people talking what sounds like utter gibberish, yet making complete sense to each other never fails to entertain.
When taking this gentleman to hospital I drove past six known drunks in the space of one street. Alcohol and alcoholism is a big blight on our society. On some shifts the only jobs we have are those influenced in some way by alcohol. Most assaults can be attributed to alcohol, frequent callers (sometimes 6 times in one day) are very often alcoholic, and the amount of ‘collapse ?cause’ jobs that turn out to be drunks is frankly astounding.
My personal view (and not the view of the LAS by any means) would be to prohibit alcohol, but legalise cannabis. Not only would it cut our workload by, at my estimate, 60–70%, but I’ve never had anyone high on cannabis try to hit me. Cannabis users are very rarely violent, tend to be generally easier to handle and seldom get loud and annoying. It’s true that there are long-term health consequences, and that heavy ‘stoners’ can waste their life away, but the same holds true of alcohol and alcoholics.
On the rare occasions that I get called to someone on cannabis, it’s normally because it is their first time and they feel ‘dizzy’. Often a pat on the head, and an explanation that this is what is supposed to happen is enough to calm them down, and they will rarely require a trip to hospital. Because the intoxicant effects are fairly self limiting, people tend not to overdose on cannabis, unlike alcohol (which is why you find drunk people collapsed in the street).
There is one problem with the use of cannabis – I’m never sure what to call it in order to sound ‘hip to the kids’, the slang just befuddles me. Is it ‘green’, ‘pot’, ‘hash’, ‘reefer’ or ‘draw’? At least alcohol is just ‘booze’.
And now the government has made it even easier to get hold of alcohol with extended ‘open hours’. Oh well …
Too Quick?
(What I’m going to post about might come across as being heartless, or myself being lazy – I don’t think I’m either of them, but if you disagree with this post, as always, feel free to visit the blog and leave a comment.)
Tonight we got called to a residential home for an 87-year-old female with ‘difficulty in breathing’; once again it was way out of our area of coverage, but we made good time to get there. I’ve been to this home before, and it is one of the better ones I’ve visited; the residents are always clean, and appear well looked after. The care staff know their ‘charges’, and are always friendly, helpful and courteous towards ambulance crews.
I knew there was something wrong from the face of the member of staff who met us. She had a look of total concern, and I don’t like to see that look on someone’s face – it never bodes well. We went through the clean corridors and busy lounge of the home into one of the residents’ rooms. There were three nurses there, one of whom was crying (something I don’t think I’ve ever seen before); lying in the bed was a little old lady who was extremely close to death. Her pulse was weak, and thready, something I could have guessed by the patient’s colour. I very quickly told the staff that, yes, she was extremely ill and that she would have to go to hospital unless she had a ‘Do Not Resuscitate’ order. The staff said that it would be best to take her to hospital. We scooped her up, and her heart and breathing stopped in the lift to the ground floor.
I don’t believe in a ‘slow blue’ (where CPR is performed by ‘going through the motions’ knowing that the patient will not survive and that the CPR is for the benefit of the relatives), so I started active, aggressive treatment while my crewmate drove us the 5 minutes to hospital. The patient remained in asystole (no heart activity at all) and on reaching hospital the doctors there declared her dead.
I may have previously mentioned the study that showed that ‘out of 185 patients presenting with out of hospital asystole arrests, none survived to be discharged’. Both my crewmate and myself – and the hospital staff – knew that this patient had no chance of survival and that the reason we started CPR was because of our policy to commence resuscitation except in certain tightly defined circumstances.
If we had got there a minute later, the patient would already have died – in her bed surrounded by people that cared for her (although not her family) as opposed to being hoisted out onto a chair and then suffering the indignities of CPR in the back of an ambulance. While trying to resuscitate her during the transit to hospital I found myself looking into her dead blue eyes, apologising to her and hoping that she couldn’t feel anything that I was doing to her.
I don’t know if it is because I’ve had one and a half hours’ sleep in the past 38, but it made me feel bad to put her through the indignity of pointless CPR. I know the policies are there to protect us (and members of the public), but sometimes I wish we could use some discretion.
Now I’ll see if I can get some sleep.
I can still remember her sparkling blue eyes looking up at me.
From One Extreme …
So, two nights ago I was dealing with death, people collapsing on the DLR (Docklands Light Railway), young men vomiting blood and looking like death warmed up, and women having miscarriages. Basically everyone I attended to on Wednesday night needed an ambulance.
Last night we had …
One patient with indigestion (for 2 years – FRU on scene when we got there as it was given as a ‘chest pain’).
One ‘gone before arrival’ (a drunk who phoned 999 complaining of a broken arm, but had wandered off before we got there).
One overdose ‘acting violent’, who also had gone before we turned up (driven to hospital by her brother).
One ‘facial injury’ (a woman slapped by her husband: no injury and she didn’t want to go to hospital – her husband was taken away by the police).
One patient with ascites and chronic alcoholism, who was referred to hospital by the GP (could have travelled in her husband’s car).
One call to a police station for an accused who had swallowed some drugs – he denied everything and the police doctor cleared his health.
And one patient with an arthritic knee …
The patient with an arthritic knee was a 70-year-old male who had called out his GP. Said GP had then diagnosed arthritis and decided that the patient needed hospital treatment. We got the call, and had to go out of the area we are supposed to be covering to pick the patient up. The booked hospital was even further out of our area – so much so it was in another sector.
When we got there the patient’s son was present and as we loaded his father into the ambulance we were told that ‘I’ll follow up in the car’.
The look of sheer despair my crewmate gave me had me in fits of laughter; thankfully, I was outside the ambulance so neither the patient, nor his son, who had gone to get the car, could see me.
There was no reason why the patient couldn’t have been driven by his son, yet here we were, out of area, going even further out for someone who didn’t need an ambulance.
Still, after the past few days it was nice to have a shift where no-one was actually ‘ill’, and so we could spend the shift in a fairly relaxed state.
We often get patients in this sort of situation. I’ve given up worrying about it, even if it does mean that an ambulance is tied up doing non-essential work. I just wonder how many people have died because of a delay getting an ambulance because we are forced to do these types of jobs.
Driving for the LAS (For Dummies) Part 1 (Assessment)
When you apply for a job as ambulance personnel for the LAS, one of the things that they look for is that you are a competent driver. Therefore, as part of the interview process they throw you into the most run-down, barely working 14-seater lump of crap they can find, and tell you to drive around Earls Court. For those not from London, Earls Court is a congested area with fairly small streets, constant roadworks and the sort of people who think it is amusing to leap out in front of scared-looking interviewees on their driving assessment.
Before you see a vehicle you are given a piece of paper that tells you what the assessor is looking for, the crossing over of hands when steering is a big no-no, as is over-confidence (along with under-confidence), speeding, going too slow, incorrect use of gears, incorrect use of signalling and a myriad of other things you haven’t worried about since you passed your driving test as a teenager.
When I first went for my driving assessment I noticed the ‘over-confidence’ bit, so I thought I’d be sure not to come across as too aggressive a driver. I was a model gentleman, I let people out of side turnings, allowed pedestrians to cross in front of me and didn’t hassle people who were driving too slow: I failed my assessment for being ‘under-confident’. ‘Come back in 3 months’ I was told.
Three months later and I was determined not to make the same mistake (an additional 3 months stuck in A&E nursing will make you ever so slightly determined). So, I got into the worst piece of crap in the fleet, and off we went. Leaving the yard I hit a kerb and about 200 yards down the road I did the same thing. ‘Turn around and go back’ I was told; I slunk back to the yard and vowed to do better in another 3 months.
Three months later, and I thought ‘Sod it! I’m going to drive how I normally drive’. So I crossed my hands turning the wheel, sped up to stop signals, refused to let anyone out of a side road and drove as if I were driving my 1.0-litre Ford Fiesta.
I passed. Needless to say I was more than happy, and fairly skipped out of the yard that morning.
Of course this double failure didn’t help my confidence when it came to the driving part of my training course.
All I can say is that I haven’t run over any pedestrians, although I have reversed into some stationary objects.
Driving for the LAS (For Dummies) Part 2 (Training)
When you train to be an ambulance technician, you have to do 2 weeks of ‘driving instruction’ where you are split into groups of four, get given a 17-seater van that has been hired for you and you learn how to drive your ambulance using this equipment.
Perhaps the most important differences between an ambulance and the 17-seaters that we are given are that ambulances are automatic, while the 17-seaters are manual (I believe the American term is ‘stick’), and that 17-seaters just don’t ‘feel’ like an ambulance.
The training course consists of 2 days of fun, and the rest is chasing each other around the countryside at high speed.
The two days of fun include driving around a racing track, spinning around a skid-pan and swerving around traffic cones at high speed – both forward and in reverse.
Then, for the next 2 weeks, you learn some theory in the classroom, such as the ‘limit point’ and the forces that act on a vehicle (and why sometimes speeding up when you are losing control is a good thing). The rest of the time is spent driving at high speed around the countryside, making sure that you have the correct gear, speed and suchlike for high-speed cornering.
There are a few things that make this training course less than effective: the first is that as the London Ambulance Service, it is extremely rare that you find yourself driving in the countryside, it is also rare that you drive at any speed above 40 m.p.h. and, as mentioned earlier, ambulances are automatic vehicles and as such don’t have gears.
I drove an actual, real ambulance a grand total of once during training. I sat in the driver’s seat, pointed to the lever in the middle of the floor and said, ‘what’s that, and where is the clutch pedal?’
Luckily for me learning to drive an automatic was pretty easy.
At no point during the driving course did we drive on ‘blue lights and sirens’ – something that may have caused my first RTA.
(Insert wobbly flashback special effect here …)
The first day out on the road out of training school went well. I was attending (A&E nurse for some years) and my crewmate was driving (his previous job? ‘Man and Van’ – driving a removal van around London doing odd jobs). So the driving went well, as did the attending (dealing with sick people). The next day our roles were swapped, I warned our supervisor that I’d never really driven an ambulance before, but he said that we’d be fine if we worked like yesterday.
So, on my first emergency job, blue lights went on, sirens went on and people started moving out the way – it was then that I realised that you can’t fit a 7-foot-2-wide ambulance through a gap made by two cars which is only 6 feet and 6 inches wide. This was the first time (and hopefully the only time) I’ve been sworn at by a boss, although to be fair, the only time I think I’ve deserved it. I learned how to fill in accident forms that day … and how to judge distances a bit better. (An ambulance is wider, longer and taller than a 1.0-litre Ford Fiesta.)
Soon my training came to an end and I was thrown into the world of emergency driving in Newham …
(End wobbly flashback sequence, cue end title ‘To Be Continued …’)
The boss who swore at me was right though. Even now I think that this is why I like the ambulance service over nursing. With nursing the boss would call you into the office to discuss your ‘problem’, and how I might ‘reflect on what happened’. So for me, being sworn at was a breath of fresh air.
Driving for the LAS (For Dummies) Part 3 (The Real Deal)
After the assessment, the training and the first time racing around the streets of London being sworn at, you finally end up on your own, in a new part of town where you are expected to get to emergency calls in 8 minutes.
I got posted to Newham, which is a 10-minute drive from where I live; unfortunately, I’d never driven there and my navigation was awful. When I told my new workmates where I lived they thought, ‘Good someone who knows the area’ (and just after that they probably thought, ‘If he lives there I wonder if he’ll steal my car?’). This was before the days of satellite tracking where you just have to follow the dulcet tones of the computer (sometimes in Danish if some bright spark has reprogrammed the computer); in those days you had a mapbook and were expected to get on with it.
Gradually, you get to know the streets, where the regulars live, the pubs that are ‘trouble’ and where the 6-feet-6-inch width restrictions are. You then have to counter every threat the ‘natives’ throw at you.
For example, I might be driving a big white (or bright yellow) van, covered with flashing lights and ‘ambulance’ written on the side, occasionally – if I feel like pushing out the boat – I’ll even have the sirens going. You might expect people to get out of the way; instead, pedestrians will be drawn to run out in front of you, like particularly dim-witted moths to aflame. People in cars will suddenly develop selective blindness, and idiots with Drum ’n ’Bass pounding out from stereos worth more than their car will argue that I should make way for them.
Drivers will pull out from side streets in front of you, and as for the bizarre ideas some people have as to the best way to clear a path for us (jump on the brakes, swerve in front of us, sit there and panic), well, it’s a good job we often don’t have far to travel.
However, there are benefits to driving an ambulance: driving on the wrong side of the road (at a top speed of 20 m.p.h. mind you) still makes me happy, driving over kerbs is often a giggle, and let’s face it, who wouldn’t like to treat red lights as a ‘Give Way’?
Despite popular belief, we don’t actually go that fast – we can’t, we never know when some young mother is going to push her baby buggy out in front of us. At best I think we have a maximum speed of 40 m.p.h., not only for our safety and the safety of other people, but purely because the worn-out ambulances that we drive have an acceleration that would embarrass a milk float, and a top speed of … oh … about 42 m.p.h.
I once got on a motorway and ‘opened her up’, we got up to 70 m.p.h. (downhill naturally) before the front of the ambulance started lifting up and the steering became a trifle ‘unresponsive’. Luckily I managed to stop screaming in sheer terror for long enough to regain control.
Most of our accidents (as a firm) come from reversing, I’ve – cough – occasionally reversed into pillars and lampposts; one person I worked with managed to reverse into a low-flying balcony. I have on at least two occasions got stuck in a width restriction (I swear, one day I’ll get our 7-foot-2 ambulance through a 6-foot-6 restriction – I just need to get up to a decent speed before tackling it). Thankfully, our ambulances are so old and battered that small amounts of damage just add to the character of the vehicle.
Of course all that has changed with the new yellow Mercedes Sprinters. Or at least it would if they haven’t all started getting faults around the 5 000 mile mark. Our station had three of the new ambulances, now we have none. They are all either being patched up, or shipped back to Germany to have major repairs done. Current reports are that the fibreglass back is splitting from the metal chassis – possibly because of the number of speed-bumps we have to contend with.
Speed-bumps – a good idea in theory, but in practice they slow us down by a hell of a lot, wreck the ambulances, and in 5 years’ time I intend to go on permanent sick leave because my kidneys have been shaken out through my mouth. My plan to get local councillors thinking a little more sensibly about speed-bumps would be to strap them down on a spinal board and drive them through the streets – I think they would be begging for mercy after 5 minutes.
Parking is a nightmare in Newham as well. We often have a line of traffic parked on either side of the road, making side streets effectively single track routes. When we get a call for a ‘chest pain’ (you know, the sort of thing that could be a heart attack), then we have no choice but to park in the middle of the road, blocking any other traffic. At no point do we engage in the ‘how much traffic can I stop’ game. We don’t like confrontation at all, we like a nice quiet life, so we are not trying to wind people up on purpose.
Unfortunately some people don’t see it like that and will sit there honking their horn at us to get a hurry on. To be fair, I tend to spend a maximum of 10 minutes on scene, and if you honk your horn at me, I’ll then change my working speed to ‘go slow’ (assuming that this won’t affect the patient’s condition).
I think it’s incredibly rude to think that your journey is more important than that of an emergency ambulance.
Don’t you?
I’m off to work now to drive around those selfsame streets … wish me luck, and if you see me in your rear view mirror, please get out of the way by pulling over and stopping on the left of the road.
Bombs, Bongs and Dive-bombing
Some unusual jobs today, the first call was to a concrete company (which will remain nameless – no doubt they have better lawyers than I). We were told to meet with the Police and Fire Service at an RVP (meeting point). It turns out that some animal liberation types have taken offence to this company (rumour being they are supplying concrete to a new animal testing laboratory) and have sent some deactivated incendiary devices to various branches in order to scare them. Today, in three of the offices across London, some ‘suspicious packages’ had turned up and we were being sent to cover the defusing of one of these devices. Two ambulances, one Duty Officer, three fire engines and countless police were there, standing around the now evacuated offices.
Our Duty Officer started allocating ‘Major Incident’ roles to everyone. I don’t think he was best pleased when I asked him why, when major incidents are designed to deal with multiple casualties, we needed to play that game when the only person in any danger in the now deserted office was the bomb disposal officer.
He sent me to arrange the parking of the emergency vehicles. We were soon stood down, however, when it was discovered that the ‘device’ was actually a packet of envelopes.
The next call was to two brothers who had fought over possession of a bong, with one brother trying to sell it to a third brother. Both we and the police were sent; when we got there both brothers had calmed down and there were no serious injuries. One policeman was confused about what a bong was used for, until I explained that it was ‘drug paraphernalia’. One of the brothers told the policeman that he was selling it because he didn’t use it – he much preferred smoking his cannabis in a spliff.
Luckily for him the policeman ignored this massive blunder (and me collapsing in tears of laughter at this idiot essentially confessing his drug habits).
Our next interesting job was to a man in Docklands who had a head injury caused by trying to avoid an attacking seagull. It turns out that there is a seagull living there who likes to dive-bomb people passing by. This man had ducked the avian attack, then tripped and fell flat on his face, knocking himself out. He had only minor facial injuries, but the loss of consciousness will mean a short stay in hospital being watched. My old crewmate suggested that he sell his story to the newspapers.
The rest of our jobs were rather boring after this early excitement.
Shouldn’t You Be Dead?
One of the things that will constantly amaze me is that some people will drop dead at the drop of a hat (so to speak), while others will survive injuries that would kill us mere mortals.
Today was a case in point: we got called to a 39-year-old female who’d been hit on the head by a brick that had fallen seven floors. We turned up at the location fully expecting to see someone with less of their brains inside their head than would be considered healthy. Instead, the woman was sitting in a chair (having had a C-spine collar applied) with her head supported by a BASICS doctor (a doctor who volunteers to respond to calls in the community).
This woman, who should have been dead, had a 1-inch cut on the top of her head.
… And that was it.
The brick had hit her on the head, then had hit the floor with such force that it had shattered. Yet, here she was with no injury other than complaining of the cut being painful. There was no loss of consciousness, but we treated her as if she had a neck injury, purely because of the ‘mechanism of injury’. It’s been a while since I’ve had to do a ‘standing take-down’ (where you get a standing patient onto a spinal board by placing it against their back and laying it flat with them on it) but it all went smoothly, the doctor travelled with us and was a pleasure to work with.
Although she was 39 the woman actually looked like she was in her early twenties – perhaps she has some witchy super powers? Either way she was discharged later in the day.
She was exceptionally lucky – if you can call getting beaned by a brick ‘lucky’.
Crunch … Crunch … Crunch … Masked Symptoms
I discovered yet another reason to avoid alcohol, namely that it can mask the symptoms of otherwise obvious illnesses and injuries.
We got called to a 60-year-old man who had fallen in the street: as it was 2 a.m. we could guess that alcohol was involved. When we arrived on scene the patient was standing against a wall very much the worse for drink. Admitting he was an alcoholic he told us that he had tripped over and now his right leg hurt. While he was standing there I gave him a quick examination, he had no bony tenderness and was able to bear his weight on his leg. He could feel his toes wriggling in his shoe and there was no obvious deformity to the leg. We helped him walk the few steps to the ambulance, but he was unable to manage the stairs at the back of the ambulance so we put him in our carry-chair and lifted him into the ambulance. Further examination showed little else of note; his pulse was a tad on the high side but otherwise his blood pressure and other observations were well within normal limits.
We transported him to hospital, where the nurse gave him a quick examination, essentially repeating the examination I’d given him in the field, and she sent him out to the waiting room.
When we returned to the hospital a little later we were told that he had a fractured neck of femur – essentially he’d broken his hip.
He was so drunk that he felt little pain, and for various reasons none of the normal signs of a broken hip were present. Luckily, I’d documented that I’d examined for the possibility of this type of fracture and found negative signs all the way along, so should he complain (which I doubt he would do) both I and the admitting nurse would be covered.
So … don’t drink, or you may find yourself walking around on a broken leg.
Now I’m off to sleep. Two very long night shifts and I’m ready to collapse.
It’s one of the main differences between A&E nursing and ambulance work – in an A&E department you have good lights, can undress the patient and can put them on an examination table. In ambulance work you can find yourself down dark, unlit streets, in the rain and with the patient lodged under a car. I did feel a little bad about this patient, mind you …
An Excellent Bad Day
Have you noticed how much I talk about being tired or needing sleep? The benefits of shift work …
First off, I’m bloody knackered, frazzled, chin-strapped, and generally tired. If I ramble just poke me in the ribs with a stick.
Today was both bloody awful and rather good fun, which despite sounding like the ramblings of a madman is a perfectly sane way to describe today, although I’ll be glad for it to be over.
The day started badly: I woke 3 minutes before my alarm was due to go off so I turned it off and woke for the second time 10 minutes before my shift was about to begin. I didn’t get much sleep last night so I suspect my body overruled my brain to give me an extra 50 minutes of sleep.
Luckily, when I wake up with an adrenaline jolt like that I can get washed, dressed and speed through the streets of Newham like an Olympic sprinter on methamphetamine.
Turning up at the station I found out that my regular crewmate was ill, and instead a ‘Team Leader’ was being sent to work with me. Team Leaders are on the lowest rung of management: they are the people who are supposed to keep the troops in trim, and so spend considerable time moaning about the speed at which we get to jobs, and the poor quality of our paperwork. I’m of the belief that if management don’t know about me, I can’t get in any trouble, so working with a new Team Leader was something I was less than happy with.
I had barely gotten to say hello to ‘Team Leader’ than we got our first call of the day, a ‘Suspended’ (cardiac arrest) a couple of miles from station. Manoeuvring a big yellow taxi through rush-hour traffic is no fun at the best of times, but as I was driving I gave it my best shot – we got to the scene shortly after our First Responder who was already bagging and giving CPR to an obese woman in her eighties. As we were in one of the new yellow ambulances I lowered the tail lift, got the trolley out and nearly ruptured myself lifting the patient onto the trolley bed. Rolling her out to the street, we got her on the tail lift and raising it, rolled her into the back of the ambulance. All that was left was for me to raise the tail lift the rest of the way and rush to hospital.
You may notice that I spent some time discussing the tail lift; this is because as I went to lift it, the hydraulics failed and it was stuck, sticking 7 feet out from the rear of the ambulance at a height of about 4 feet from the floor.
I gave it a kick, a shake and then resigned myself to manually lifting the bloody thing up, all while the crying relatives were watching me pumping the manual handle like an idiot. Finally, it was raised to the closed position, so I made my way rapidly to hospital while ‘Team Leader’ and ‘First Responder’ worked on the patient in the back. I’ll not mention the road closure that forced me to make a painfully wide detour, but otherwise we reached the hospital with some speed where the woman was, unsurprisingly, declared deceased.
After a quick tidy-up of the back of the ambulance (which after a cardiac arrest always looks like a bomb site) we got a job to an ‘unwell child’. The 15-month-old child was indeed unwell, although not life-threateningly so. The assessment was made harder by the mother having very poor English and the child having ‘Development Delay’, which encompasses a multitude of syndromes and genetic/biological causes.
The next job was a transfer from the local maternity department to a maternity department in another county. This is a hospital that I had no idea how to get to (the details of why there was a need for transport are too boring to go into; also, I think I might say something about the mother I’d regret in the morning). I set our travel computer to give me directions to the hospital and we set off. The journey was supposed to be 9.8 miles, but after following the computer’s directions to the letter we had travelled 37 miles along rather crowded motorways.
We had taken 30 minutes longer than we had planned. It’s the last time I trust that bloody machine. ‘Team Leader’ was not happy about the computer but we laughed it off.
The next job was a simple maternity which we drove into the London Hospital. This was fine until I managed to drive into another ambulance when trying to leave the hospital. No damage to my ambulance, and minor damage to the other, but as my first accident in over 18 months, it was obvious that it would happen when ‘Team Leader’ was sitting next to me …
Returning to fill in the accident paperwork, Control asked us to attend to another call – this time it was an obese unconscious 70-year-old female. She was extremely heavy and, because of her ‘floppiness’, was a complete dead weight. Once more I nearly killed myself lifting her. All her body functions and observations were normal so it was a complete mystery why she was unconscious, although I could confirm that she had been incontinent of urine …
… after I put my arm in it.
All these problems throughout the day meant that we worked harder than we needed to – and yet, throughout the day we had a great time as we laughed and joked between patients and vowed never to work together again. I said that I’d take sick leave, saying I was ‘stressed’ and ‘Team Leader’ said she would make sure I got sent to the other side of London before she worked with me again.
And so, at the end of the shift we parted, laughing at the thought that it was possible we could be repeating the experience tomorrow.
I’m looking forward to that possibility.
‘Team Leader’ is still on our complex and is still a good laugh. Thankfully, I haven’t had to work with her again.
Broken Ambulances
One of the main problems with the LAS at the moment is the lack of vehicles. In the past this has come to mean that there are not enough staff to man the vehicles that we have, or fill the rota to maintain safe cover over our area. Lately, however, we haven’t had the vehicles physically present. At the moment, I am typing this from work and looking out the window at the fitters whose job it is to maintain the fleet in our area of London. There are 13 ambulances waiting to be fixed. There are 3 crews sitting on station unable to take any calls because their vehicles have broken down.
Someone has just visited us in the staff car (a nice little Corsa) and, on attempting to leave, its clutch has broken.
Today I took an ambulance from West Ham over to Poplar to replace a vehicle whose steering had broken. Two management brought over a spare vehicle from Newham for me to work on – a vehicle that had just had a broken rear suspension fixed.
Let me tell you, riding on an ambulance with no suspension is an ‘interesting’ experience – you get thrown around and the cupboards fly open spraying bandages and other, less soft, equipment around the cabin.
This ‘fixed’ ambulance lasted three jobs before the suspension died again and I was bouncing around the cabin. It also stalled if you closed the choke.
So now I’m sitting on station twiddling my thumbs, unable to continue my daily grind of saving lives picking up drunks.
The fleet is just falling to bits, the new Mercedes have faults developing around the 5 000 miles mark and the tail lifts are extremely temperamental (like my experience yesterday – they fail at the worst possible moment). The LAS needs a cash injection so that it can have a fleet of basic, but reliable ambulances, fully equipped and fully manned.
Things haven’t changed much since I wrote this, although with a few extra vehicles the turnaround for crews without a vehicle is a bit better.
An Apology to A&E Departments
I would suggest that a lot of the people who read this are doctors and nurses of one persuasion or another. I also guess that many of these readers have some experience of A&E departments.
So, as an EMT I wish to apologise.
I’m sorry that throughout the shift I will continue to bring fresh meat to the grinder, that is, I will be forced to transport patients from ‘outside’ into your department, where they will need to be looked after and assessed by your own good selves.
I’m sorry that I have to sometimes bring their relatives who will harass you about waiting times, the pain their relative is in and about why you are drinking that cup of coffee while their dearly beloved is ‘at death’s door’. I’m also sorry that sometimes I couldn’t bring the only relative who can translate the patient’s moaning and groaning into English, thus making assessment a thousand times easier.
I’m sorry for the dross that I bring to you: the cut fingers, the bellyaches and the spotty backs. I’m sorry that the primary health-care workers (the GPs) are often so useless as to be a liability. I’m sorry that you have to cope with the fallout that occurs because there are so few good GPs and you have to become the first point of call for coughs, colds and diarrhoea
I’m sorry that the schools don’t teach basic health and first aid to their students, preferring to waste time on the history of glaciers or the solving of quadratic equations. This means that the population wouldn’t know the difference between a minor cut and an arterial spurt if it jumped up and hit them over the head with a hammer, neither do they know which of these two injuries warrants a trip to the local Emergency Department.
I’m sorry that our communities where our Elders teach our Youngsters and the Youngsters listen no longer exist, resulting an influx of first-time mothers who think that when a baby vomits it is a precursor of death.
I’m sorry that the protocols and guidelines that we adhere to don’t allow us to leave patients at home. In England at least, we have to transport to hospital. The government thinks that we cannot tell the difference between serious cases and the aforementioned cut finger.
I’m sorry that the police cannot look after drunks on a Friday night; they worry that they will choke to death in the cells, and so we get called. We have nowhere else to take them to but your department. Sorry.
I’m sorry that I bring in those serious cases 5 minutes before your shift finishes. If it’s any consolation it’s probably 5 minutes to the end of our shift that people decide to have their heart attacks, their amputations and their dissecting aortic aneurysms. Like you, this means we get off late as well.
I’m sorry, but it’s not my fault.
I wrote this in part because we do sometimes get dirty looks from A&E staff as we drag in the umpteenth drunkard of the shift. It’s not my fault that the government made 999 so easy to dial.
Knee Trouble
Gillick competency is the ability of youngsters under the age of 16 to give informed consent for medical treatment. Essentially, we have to assess whether a child is competent enough to make decisions about their own body. This is, as you might guess, an ethical minefield.
Back to work with the rather enjoyable 18:00–01:00 shift, where you tend to get lots of drunks, and very few serious cases that require me to do some actual work.
However, you do occasionally come across a job that is tricky, not because I worry about the patient’s illness, but instead for reasons that to the non-ambulance person are hard to understand.
Our first job of the day was one of those very jobs. The call we were given was 13-year-old female with a dislocated knee. Nice and easy I hear you say, but lots of minor problems can build up to make a job less than ideal.
We arrived on scene and found a patient who had a rather obvious dislocated knee – just imagine your kneecap shifted 2 inches to the left, so much so that it casts a shadow on the rest of your leg. Simple enough to deal with: if you are feeling brave you can slide it back into place yourself, or go the more recommended route which is to take the patient into hospital and let the doctors fiddle with it.
Then the problems started piling up. To start with there were no adults present, just another (unrelated) teenager; neither the patient nor this other teenager were what you would exactly call brain surgeons. We are not supposed to deal with children without an adult present, but what else can you do in those circumstances? The father had been called, but he was travelling from another hospital where he had been undergoing outpatient treatment. So we had to decide whether it was ‘safe’ for us to take the patient to hospital – we use ‘Gillick competency’, but it’s always a bit of a gamble on our part.
The patient had fallen from her bunkbed so her friends (who had run off) had lifted her back onto the top bunk. She was screaming in pain (which is fair enough I suppose), and wouldn’t let us near her. This little problem was solved by giving her a lot of Entonox (known to some people as ‘laughing gas’). After enough of this stuff she started laughing and we essentially ‘grabbed’ her off the bed.
Then she refused to sit in the carry-chair, but because we were upstairs she needed to go in it. After a lot of persuasion, and a lot of her screaming very close to our ears, we managed to get her to sit down; this had the rather excellent side-effect of popping the kneecap back in place.
This would normally mean that the amount of pain goes down by a lot, but this girl had a touch of ‘hospital phobia’ so she continued screaming. While screaming she was also arguing with the teenager who was with her, telling him that he needed to come to hospital with her but he was refusing because ‘How am I gonna get back home?’ I must admit I really wanted to tell him to walk it, because the hospital was only about 1 000 yards away. Despite her pleading with him, he wasn’t for budging. He set his Burberry baseball cap square on his head and refused. I don’t think she is going to be too happy at him next time she sees him.
Once that argument had run its course (and my crewmate and I managed to stop laughing), we had to get the patient downstairs – this was made more difficult by a sideboard that was in the upper hallway by the stairs. To counter this problem, we had to lift her completely over the banister. Luckily she was a lightweight, and my crewmate and I are – cough – both strapping, good-looking men.
We saw her later in hospital, having a plaster cast put on her leg, so that the kneecap wouldn’t slip out of place. She was much happier and surrounded by her parents. She even managed to give us a smile, which, in the end, made the job worthwhile.
So, this is what we occasionally have to deal with, not so much the life-threatening stuff, but more the silly little things that can make an ‘easy’ job much trickier.
Drunk and Disorderly
We got called to a pub (which is always promising), to a 24-year-old female who was having ‘difficulty breathing’. When we turned up at the pub, we were met by a man who, after letting us know he was a ‘first aider’, told us that she was fitting and that she had stopped breathing, but that mouth to mouth resuscitation had ‘brought her back’.
Entering the pub we found the woman thrashing around on the floor. She wasn’t having a fit, it was more like a temper tantrum. Throwing himself on top of her was her husband, who was reluctant to let us approach her. People in the pub told us that they had both been drinking heavily.
We near enough had to force the man off of his wife just so we could examine her properly, and it soon became apparent that she was just very, very drunk. Out of the corner of my eye I saw sudden movement and ducked quickly as the husband threw his wife’s shoe at a man standing behind me. We decided that loading her onto the ambulance would be the best thing to do. The husband demanded to be let in, but we told him that we needed room to properly examine his wife. He banged on our windows twice, but then left, apparently running up the road – possibly as a result of him throwing a pint glass at another of the pub’s customers. (This was very unwise of him, because half of Newham police force were 200 yards up the road dealing with an armed incident.)
By this time a second crew had turned up, as someone had called 999 and told our Control that the woman had stopped breathing. We stood them down, although, on reflection, they could have been of help keeping the woman on the trolley because she was still throwing herself around, refusing to lie still, and generally making life difficult. We managed to get a blood sugar, pulse and blood pressure (all of which were normal) but she refused to stay on the trolley and wouldn’t sit on a chair – so we let her lie on the floor.
At times like these, I think I’d give my eye-teeth to be able to put people like her in a 4-point restraint, but it’s something we are not allowed do.
Later, while I was driving to hospital, she made an attempt to leap out the back of the ambulance, and it was only the rugby skills of my crewmate that prevented her escaping under the wheels of a following car. The rugby tackle was all the more impressive given that my crewmate is 5-foot-nothing tall.
We finally managed to get the patient to hospital, where she threw her vomit bowl (with vomit) over the floor and tried to hit a nurse. Luckily I was standing behind her and grabbed her before she could damage any of the staff, or even a patient.
To cut a long story short, the nurses let her phone her sister to come and pick her up, and then kicked her out the department.
Two things about this job that bring a smile to my face: (1) one of her shoes is still lying in the gutter, where we picked her up from, and (2) her husband got out of prison today and, given his attitude and behaviour, he’ll soon be back inside.
So, it’s not just weekend nights we get the violent drunks, it’s every damn night …
We are not taught how to restrain patients who might be violent but sometimes it is essential – for example, in the event of someone having a serious head injury and becoming violent. So, we have to make it up as we go along and hope that it turns out alright.
Favourite Job
The other night I had my favourite type of job, the type of job that meant I wasn’t upset to be late leaving work.
People who are diabetic sometimes have very low blood sugar; this makes them confused, agitated and sleepy, and this can lead to unconsciousness and even death. Their blood sugar can become low for any number of reasons. Most often they have done more exercise than normal and not eaten enough to raise their blood sugar.
The treatment for this condition is to either give them sugar or an injection that ‘frees up’ some sugar that is stored in their liver.
Our patient last night normally controls her diabetes very well; so much so that her family had never seen her with a dangerously low blood sugar (the medical term for this is hypoglycaemia). They called us because she was acting confused and was unable to speak properly or stand upright. We arrived, and found out she was a diabetic; checking her blood sugar we got a reading of 1.6 mmols (the normal range for a diabetic is around 4.5–12.0 mmols) – this is very low and explained why she was losing consciousness.
The family were understandably upset, as they had never seen this before. They saw her slipping into a coma in front of our eyes, so we explained what was going on as I prepared the injection that would raise her blood sugar. I gave the injection (this injection is called glucagon) and waited for it to take effect, all the time reassuring the relatives.
Within 10 minutes she was up and talking, we then gave her some sugar jelly which raises the blood sugar some more. Soon she had made a full recovery, with her blood sugar reading 5.6 mmols. We gave her some carbohydrates (for ‘slow-burn’ energy) and left her in the care of her exceptionally happy family.
The reason why this is such an enjoyable type of job is that we are actually saving a life (for a change) with the treatment that we can give, and that the recovery is normally rapid, and always impressive. From unconsciousness to 100% fitness in the space of about 15 minutes really impresses onlookers … and it does our ego good to be praised every so often.
Notting Hill – Stabby, Stabby
Yesterday was the last day of the Notting Hill Carnival. The police are calling this year’s carnival a success, with little reported crime, but I would tend to disagree: it’s just that the crimes all happened to people as they travelled home.
Our second call of the night started worryingly when Control told us that a male had been stabbed in Stratford shopping centre, and that he could still hear shouting in the background of the call. The stab vest went on and we made our way down there, meeting up with a lot of police officers trying to control a rather large crowd of post-carnival spectators.
We found a 15-year-old male lying on the floor, with a policeman holding some paper tissues over an upper abdominal stab wound. There was no external bleeding, and the patient was alert, calm and talking. He also had a small wound to his right leg, which again was not bleeding significantly. I ran through a primary survey (a very quick examination of the patient to rule out anything that is going to kill him in the next 5 minutes) and then concentrated on making sure his chest and lungs were not damaged. On clearing them I turned my concentration to the belly wound.
We don’t like stab wounds: they can do a lot of damage leaving only a tiny entry wound. One stab wound can easily kill you, whether it is in the leg, the arm, the chest or the belly. After my examination I decided that, although he needed exploratory surgery, he wasn’t critically ill. There was a bit of ‘something’ poking out of the wound, I had no idea what it was (I initially thought it was part of the policeman’s dressing) so I soaked one of our dressings in saline and applied it to the wound. We then got a phone call from what I took to be the HEMS road team (a doctor and paramedic) letting us know that they would be on scene in 12 minutes and that the patient should go to the Royal London Hospital. The problem with this is that the Royal London is some way further away than Newham, and that I knew that if the HEMS crew got on scene they would want to ‘stay and play’ securing IV (intravenous) lines, considering intubation and running a full examination on the roadside. In my opinion, having assessed the patient, his best option would be to go immediately to the nearest hospital and let the surgeons there deal with him.
So, we loaded the patient onto the ambulance and made a run to Newham hospital which took us less than 5 minutes.
The result of which was the patient got to theatre, was ‘packed’ as he had a lacerated liver and gall bladder and is now in ITU for recovery.
I wonder if the HEMS crew will moan. I suspect they won’t because around the corner was another young lad who had been stabbed in what later turned out to be a connected series of battles between two schools. The HEMS crew played around on scene with that patient before taking him to the Royal London Hospital (who really love their trauma jobs). There were then reports throughout the night of other crews picking up more teenagers injured during the fight. The patients were spread fairly evenly between the two hospitals, so no one department became overloaded.
A couple of things struck me as amusing, the first was that when we were about to leave for hospital the patient’s girlfriend and cousin were fighting amongst themselves over who loved him more and should go to hospital with him. The patient’s brother was also there and was fighting with police to get to the patient. He then vanished, and my prior experience would suggest that he was planning revenge and a counterattack.
While going to hospital, the patient’s girlfriend was talking about the other lad who had been stabbed (apparently his name is ‘Biggy G’) and how it seemed that the fight had been planned at the carnival.
As always when I got to the hospital it seemed that the doctors weren’t interested in my handover … on which I will post/moan more later.
As we were going to hospital another crew, this time in North London, were putting in a priority call to their local hospital. They had two young men (aged 19 and 20) who had been stabbed, luckily in a non-serious manner.
A night full of people getting stabbed. Just a coincidence that it is the last night of Notting Hill? The media said that the carnival passed without serious incident. Either they were not looking very closely, or they decided not to report the violence around the capital.
Sad Stories That Stay With You
Some jobs will just make you sad, and it’s those that you’ll find yourself carrying around with you for a time. It isn’t always the death and horror that affects you, and you can be surprised by the things that haunt you.
We got a call to a block of flats, it was given as a 69-year-old female who was unresponsive and who had a history of schizophrenia. Her condition could be caused by any number of things, so you carry all the equipment up the flats as you never know what you are going to encounter.
We were met by the woman’s husband who led us through to the bedroom where our patient lay. She was on the bed and was not talking to anyone; with one hand she was ‘fidgeting’ and plucking at her clothes. This was normal for her, and could be due to the antipsychotics she uses to treat her schizophrenia. Looking at her prescription sheet we found out that she was also a diet-controlled diabetic, but her blood sugar test showed a normal amount of sugar in the blood. The patient was unable to talk, and looked very scared. Was this episode related to her schizophrenia?
Our physical exam, however, showed a complete loss of function and muscle tone down the right side of her body; this led us to think that she had had a CVA, or stroke, and that this had affected her speech and muscle function. We rapidly removed her to hospital, and, to be honest, the job itself went like clockwork.
The thing that stays with you though, is her husband telling you that they have been married for 50 years, and for the last 20 of them he has stuck by her while she was suffering first from manic depression and then schizophrenia. To have stayed by her side while she was under the shadow of these illnesses shows true love. Every so often, during the transport to hospital, her husband had to wipe a tear from his eye; he was sitting holding his wife’s hand, trying to provide some comfort to her and ease the scared expression on her face.
If she survives the stroke she will probably be permanently disabled and will require quite intensive care for the rest of her life.
I think her husband will continue to stand by her.
In unrelated news … I was so tired driving home this morning that I took the wrong turning to go home and went down the wrong street. Aren’t you glad I’m looking after the health and well-being of people?
Update on Last Posting
Lots of people want to know what happened to the lady in my previous post, so tonight I spoke to the nurse who was looking after her.
The patient continued to be unable to talk, although (perhaps sadly) she could understand everything that was happening to her, and around her. She was also unable to use the entire right side of her body. It seems that the stroke was caused by an infarct (or clot) in her brain and not the more life-threatening cerebral bleed. She went to one of the better wards in the hospital after spending some time in the Resus’ room, during which her husband constantly stayed by her bedside. The nurses looking after the pair of them felt a lot of sympathy towards them, and I think they all fell a little in love with the husband.
I mention that the nurses looked after the pair of them, because that is what good nurses do, they look after everyone affected by the illness.
Sometime later today or tomorrow she will have a CT scan of her brain to determine the extent of any infarct, and then she will start the long road to a hopeful recovery.
I used to work in a medical ward, and we would have a lot of stroke patients. Unfortunately, there is no magical medical treatment for a stroke once it has taken place; instead, it is a long gruelling slog through physiotherapy, speech therapy and occupational therapy. It can take months to recover some function, and many do not recover at all: they remain chair-or bed-bound and are discharged into a nursing/care home until they succumb to an infection that kills them.
Unfortunately, given the type and strength of the stroke this lady has had I would not hold much hope for a recovery. Miracles do sometimes happen, and I suspect that this entire woman’s family will be praying for such a miracle.
Tricky Extraction
I think I’ve mentioned on more than one occasion how, when working in a hospital, the patients are often nicely ‘packaged’ ready for examination, this can often hide the trauma that the ambulance crew has gone through in getting the patient into hospital in such a condition.
My crewmate and I got called to a ‘collapse’, and we made good time getting there to be met by relatives of a 72-year-old female who had vomited altered blood (probably from a stomach ulcer) and had collapsed to the ground hyperventilating. The woman was around 20 stone in weight (280 pounds to the Americans in the audience). She was in a bungalow, so we had no stairs to get in our way, and the relatives were willing to be helpful. The patient was lying on the floor and had just finished an episode of hyperventilation (a panic attack).
Should have been a nice easy removal, even with the weight of the patient and reduced ability to walk. We had our carry-chair and after struggling a little to get the patient on it, we didn’t expect any trouble.
Heh …
It turned out that the patient was an agoraphobic and hadn’t left her house in 20 years …
Sweating profusely, the patient fought us the entire way out of the house; she grabbed at anything tied down, at door-frames and at the handrail she had installed in her house. Trying to get a sweaty 20-stone patient out of a house is tough enough without them fighting you the whole way.
We had explained that she needed to go to hospital, and she had logically agreed, but this didn’t stop her panicking when we started to move her. When we finally managed to get her into the open air her panic rose to a dangerous level.
She was shaking, her eyes rolled back into her skull, sweat was pouring off of her and her thrashing about in the carry-chair got worse (if such a thing was possible). Both my crewmate and myself thought that she was going to have a heart attack; in fact, she had all the classic symptoms of a massive myocardial infarction (posh medical term for a heart attack). Then she started a strange screaming/moaning call that sounded completely unearthly. I could just see the next day’s newspaper headline, ‘Ambulance Crew Scare Patient To Death!’
All I could think about was to try and calm her down, so I tried using some hypnosis techniques that I just happen to know, which helped a little, but by then she was in such an agitated state that horse tranquillisers probably wouldn’t have affected her.
We managed to get her into the ambulance, where we shut the doors very quickly and made as smooth a transport to hospital as possible. During the transport my crewmate and the patient’s family worked constantly to calm the patient down, but they were only having a fairly limited success; every so often I would hear her moan in that alien fashion and my crewmate babbling at her to calm down.
When we got to the hospital, we nearly threw her off the ambulance into the A&E department; actually, she was so slicked with sweat we could have slid her off the trolley. She calmed down a bit once she was in hospital, which only made our exhausted faces seem over-dramatic to the nursing staff.
You never know what you are going to get in this job, but nine times out of ten it isn’t the illness that surprises you, but the circumstances around the job.
I can’t drive past that address without thinking about the trouble we had with that call.
Cannibals, Schizophrenics and Hermaphrodites (Oh My …)
We got called as a ‘second crew’ to an address. Sometimes, when a situation is beyond the capability of one crew to deal with, they will request another crew; normally this is because they have two patients, or the one patient that they have is too heavy for one crew to lift on their own.
We got the job as ‘female giving apple to 7-day-old baby’, which had us wondering …
As we turned up we saw the other ambulance and a police car. On entering the flat we saw two policemen standing in the corner, with a 5-foot 2-inch tall female paramedic sitting on a young woman (Patient Number 1); her crewmate was dealing with a male who had a nasty bite on his arm (Patient Number 2). The police were talking between themselves deciding what to do, as we got a quick briefing from the crew who was sitting on the woman.
It turned out that the woman (who had a previous mental illness episode), had given birth by Caesarean section 7 days earlier, and today had tried to feed the baby apple pie; she had then ‘freaked’ (note the professional medical terminology), shouting that the man wasn’t her husband, and had attacked him. The ambulance crew had been called and, as they arrived, the woman had sunk her teeth into her husband’s arm. The crew had fought the woman to – ahem – disengage her teeth, and this is why they were sitting on her. The police had been called, but were reluctant to do anything (I got the impression that they were a rather crap pair of coppers) and the second crew (us) had been called to deal with the husband (with new teeth-mark wound) and baby.
This woman was (brace yourself for more medical terms) ‘completely bonkers’, she had the rolling eyes, the delusional thoughts and the inability to communicate that separates the mildly strange from those who need immediate medication. It was actually quite sad to see this family come apart at the seams; the husband was shell-shocked, the wife was completely detached from reality and the police weren’t being very helpful (which is unusual).
We got the husband and baby out of the house and into the back of our ambulance, and then returned to see the police (finally) manhandling the woman out of the house and into the back of the first ambulance. She was securely strapped down (although we don’t have restraints, so she could have easily gotten free if she so desired); we had to lend the first crew a belt-strap as the one on their trolley was broken. The first crew then forewarned the hospital about what they were bringing in (violent schizophrenic female) and we all set off for the hospital.
We got there first and advised the nurse in charge that this was a ‘real’ warning and that security guards would be needed, along with the private ‘psychiatric’ room. It took her 20 minutes to arrange both, while the ambulance took less than 5 minutes to get to the hospital. So, while the secure room and security was being arranged this very disturbed woman was lying on the ambulance trolley … Not a good situation, and it made the job a lot harder than it should have been.
The husband was completely stunned; he had no idea how to look after a baby and quite simply couldn’t cope. Social services were informed, and the child was admitted to the paediatric ward for a while, until the husband could be taught how to look after a baby. The woman was sent to the local psychiatric unit for assessment and treatment; hopefully, this is a temporary condition brought on by childbirth (puerperal psychosis). The husband had his wound treated, and was sent home.
Oh, and the baby is a hermaphrodite.
There are jobs that you can recount around a dinner table (or at the pub) when people ask you what your job is like. This is one of those jobs, although for some reason people seem to prefer hearing about me being injured by little old ladies.
Holy Joe’s
The London Ambulance Service doesn’t just deal with emergency calls to people’s houses, we also do hospital transfers – patients who go from hospital to hospital because the original hospital hasn’t the expertise to deal with that person’s medical problems. An example of this would be the transfer I recently did from Newham to the Royal London because Newham’s CT scanner was broken, and the patient needed an emergency scan.
One of the regular places that we find ourselves transferring people to is St Joseph’s Hospice, or as we call it Holy Joe’s. Sometimes we will be picking up patients from one of the nearby hospitals, sometimes from the patient’s own home. Its one of those jobs most of us don’t mind doing. The patients are, by definition of needing hospice treatment, actually sick, and we are not so hard-hearted that we would begrudge an ambulance to someone who is ill. Then there is Holy Joe’s itself …
Holy Joe’s is a religious place, it used to be run by nuns, but now they are a bit few and far between. To be honest, I saw my first nun there yesterday, and she was picking her nose … But, you walk into the place and it just seems nice, it is clean, the staff are all friendly, the patients all seem happy and there is a really good social atmosphere there. I don’t know if it is because of its ties to the religious orders (I hate all religions, but the best nursing homes always seem to have nuns running the place), but the hospice just seems to exude calm.
My crewmate and I had just transferred a terminally ill patient into Holy Joe’s and were having a cup of tea in their tea bar (hot drinks are free to the LAS – another reason to love Holy Joe’s). Sitting in this clean, comfortable area, we were watching the patients chat with relatives, staff and other patients, giving the place a real friendly atmosphere quite unlike anywhere in the NHS. It is very rare to see a doctor sitting down with a patient, chatting about nothing in particular and having a cup of tea with them. We both agreed that this has got to be one of the better places to see out the end of your days, and that it is a real shame that there are not more places like this.
It is a shame that in this increasingly ‘technical/evidence-based/audit/professional development/governmental targets’ style of health service, we seem to have forgotten that sometimes we simply, and honestly, need to care.
I went back there for the first time in 18 months. It’s even better now. I’m thinking that the NHS should poach the board of directors and point them at some of our local hospitals.
Assaulted and Happy About It
I got assaulted yesterday, which made me smile …
We got called to ‘Male collapsed outside park’, which immediately set my ‘drunk-o-detector’ bleeping. This is the sort of call that is nine times out of ten a drunk who has decided to have a sleep in a public place as opposed to going home. In a case like this we tend to wake them up, and get them to move on before another ‘good Samaritan’ calls us out again.
We woke him up, so he stood up and started moaning that we had woken him up. Both my crewmate and myself were actually being quite nice towards him – mainly because it was towards the end of our shift and being nasty to people takes energy that we just didn’t have. Then he decided to take a swing at my crewmate, then he decided to have a swing at me … the next thing that I knew I had him in an armlock up against the side of the ambulance. My mate called on the radio for urgent police assistance, and the radio controller asked if we were both alright, to which my crewmate replied ‘I’m alright, but my crewmate is restraining him’.
The police were quick to turn up, and I had just enough time to tell them that he was drunk and had taken a swing at us before he was under arrest and carted off to the local police station. It was then I realised that in the struggle I’d managed to hit myself in the chest, right where I’ve got a broken rib. It was a bit painful. It had already gotten a whack from a heavy trolley yesterday, so I’m wondering if it will ever manage to heal.
I can tell you what went through my mind as I was pinning him to the ambulance: the first thing was ‘Oops, I hope I haven’t over-reacted’, the next thought (about 5 seconds later) was, ‘By the time I return to station and fill in the “incident form” my shift will be over … Result!’ I’d imagined that, going by the speed that the police arrested him, they were close to the end of their shift as well.
I’m just waiting for a Team Leader to read the incident form and call me into the office to ask if I need counselling …
A police friend of mine emailed me a couple of months later telling me that he had been in court providing evidence and the case before his was of a drunk assaulting an ambulance person. After a further description I could tell him that it was me who’d been assaulted. The drunk was found guilty, but had no penalty to pay as he was homeless. It would only have bothered me if he had actually connected with his punch.
Dead Babies
One of the jobs that we find ourselves going on (perhaps once or twice a day) is that of vaginal bleeding, in a woman who is around 8 weeks pregnant. This invariably turns out to be a miscarriage. Unfortunately, it is normal for the body to ‘reject’ a foetus that has no chance of developing into a full-term baby. I would suppose that this stops a woman from carrying to term an infant that would not survive outside the womb.
While dealing with such patients (some of whom have been trying to get pregnant for some time), I always try to be sympathetic, and explain that what is happening is not anyone’s ‘fault’, and that it is a normal happening.
Because of the number of people we have with this problem, and the rate at which hospitals deal with them (when working in A&E we would have about 12–18 cases of this every day), we have all become a little blasé about it. We feel some sympathy, but deep down in our hearts, we know that there is nothing we can do, and that it is a good thing that this is happening now, rather than in 6 months’ time. Nonetheless, we are worn down by the sheer numbers, and at the end of the day, perhaps we stop caring that these women are losing babies.
I have no intention of getting into the whole abortion argument, I’ve seen them done, don’t like them and would rather have the whole thing stay out of my world view.
I first thought that it was just me, and that as a male I was not best placed to pass comment. However, after having a chat with some female colleagues, it seems that they feel the same way I do, that it is natural, and that it is not worth worrying about. But it worries me a little that I seem to have come to care so little for the dead babies.
GCS 3/15 Outside the Door
There were two interesting jobs today, I’ll tell you about one now and let you wait until tomorrow for the other one.
We got called to the very common ‘Male Drunk – Police on scene’. I’ll not moan about how often we get called to this type of job, you’ve heard it all before …
We arrived on scene and were met by a policeman who first apologised before leading us to a man who was approximately 30 years old. The man was obviously drunk, and my crewmate told me that he smelt heavily of alcohol; along his arms were the scars of a ‘cutter’ – something else we are seeing more and more of these days. The policeman told us that the patient was refusing to give his name or medical details, only that he was called ‘John’.
We approached ‘John’ and he agreed to come to hospital with us. I got him into the back of the ambulance and he refused to let me touch him, so I couldn’t do my usual battery of tests. In fact, he didn’t want to talk to me at all, and sat in the back of the ambulance not talking; at one point he threatened to leave the ambulance but I managed to persuade him otherwise. (Don’t ask me why, I normally let drunks go as soon as they say they don’t want to go to hospital.)
All went as normal until we rounded the corner to the hospital, where he got off of the chair and laid on the trolley-bed. One hundred yards later and we pulled up to the hospital and I told him to get up, then I told him louder, then I did a sternal rub to wake him up – and there was no response! I then slipped an oropharyngeal airway into his mouth, this would wake anyone up, but not a flicker … he was deeply unconscious. This meant he was due for the Resus’ room.
We rolled him (rather quickly) into the Resus’ room and were met by a rather angry nurse – she wanted to know why we hadn’t pre-alerted the hospital. I explained that he had just lost consciousness outside the department. She then asked me why he didn’t have oxygen on him. Again, I repeated that he had collapsed when we were outside the hospital. We got him onto one of their Resus’ trolleys while the doctors in the department ran into the room.
For the third time I explained what had happened, and that I had no vital sign observations; this time they paid attention, and accepted what had happened.
To be honest I don’t blame them, the A&E department rarely has any surprises – the hospital is normally forewarned about any ‘nasty job’ we are bringing them, and to suddenly have a seriously sick patient turn up without any warning is always a bit of a jolt.
Now the patient was unconscious the nurses were able to do those vital observations that I was unable to do – and they were all normal. His pulse, blood pressure and blood oxygen levels were all better than mine, his blood sugar was also well within normal limits. There was no obvious reason why he was in such a deep state of unconsciousness.
He was quickly intubated, and we left the department. I’ve spent some time wondering if I missed anything – if there was anything I would have done differently – but to be honest I don’t think there was. Even if I had managed to get a full set of vital sign observations, they would have all been normal and there was nothing that indicated his condition changing so quickly. I can’t ‘assault’ a patient who has refused a procedure (such as observation taking), and all I could do was exactly what I did do – watch him while we took him to hospital.
The current idea is that he had taken an overdose of some sort along with the alcohol, and that it had started to work. Because the patient hadn’t spoken to me, I had no way of knowing if he had taken an overdose.
I never did find out what had happened with the patient – it’s one of the poor things about this job, that you can’t always follow them up.
Protecting Little Old Men from the Police?
We were asked go to the local police station to help with arresting someone. The arrestee (is that a real word?) was an 80 (or more)-year-old male who was accused of recently committing a crime that I would suggest required some amount of physical strength. We were to follow along because the person had heart and breathing problems – so much so that he had bottled oxygen in his house.
We met with the police officers (nine in total, and all rather scary looking plain-clothes types) at the police station, before following them to the address in question.
Once the police had made their entrance we were called forward to give the patient a clean bill of health. We watched as this frail man slowly dressed, needing help from his son to tie his shoelaces; we watched as he struggled around the house and wondered how he could possibly be guilty of any crime that needed any form of physical exertion.
The patient’s son was also a bit put out by the allegations, and promised to have a good laugh at the police’s expense when the truth came out.
Throughout the arrest the police were polite, helpful and behaved in a thoroughly professional manner at all times.
The patient/arrestee was also calm throughout and the whole thing went, as far as I could see, very smoothly, and our ambulance followed the car in which he was taken, until it entered the police station and the FME (Forensic Medical Examiner – a doctor that the police use) took over.
The next job we went to was to outside the same address: a woman had been mugged and the police who were searching the address had called us as she had a rather large bump on her head. Unfortunately, the mugger managed to get away. It surprises me that you can get mugged outside a house full of police and the mugger can still escape.
Victims
Imagine, if you will, getting sent to a job where a 15-year-old boy is threatening suicide. You turn up at the address and discover that it is a care home. Meeting with one of his carers she hands you a list of the boy’s medications and it reads like a ‘Who’s who’ of psychiatric drugs. You talk to the boy, and he seems calm, collected and very polite. He explains that he wants to jump out of a window and kill himself, and agrees that he would like to go to hospital. You take him into the paediatric department of a local hospital. As this does not feel like the normal ‘Teenager wants to kill themselves’ you have a chat with the children’s nurse and you ask them to let you know what happens to the patient. You leave, and continue with your shift. The next day you ask the children’s nurse about the patient and she tells you ‘The boy wanted to die because he wants to have sex with, and kill, small children – and that he knows that it is wrong’.
I hate paedophiles as much as any other member of society, but in front of me that day, I saw a victim.
Behind Locked Doors
One of the jobs that I both enjoy and hate is for a ‘Collapse behind locked doors’. This is when a (normally elderly) patient has not answered the front door or the telephone, and is presumed to be in some trouble. What we often get is someone who has died during the night. Although I hate having people die, the one good thing about this type of job is that I get to use my size 12 boots to kick down a door.
There is a skill to kicking down a door, and I was taught by the best – a policeman. The police also have a huge ram that they can use when their boots aren’t enough. These are very heavy, but also lots of fun to use.
We got called to a house where the daughter could see her elderly mother lying on the floor; shouting through the door and banging on windows didn’t get any response, so we assumed the worst. The daughter was (understandably) crying, so I had an attempt at kicking the door down.
Unfortunately for me, the woman had been burgled earlier in the year, and so had two locks, and a bolt holding the door shut, so it took a couple of minutes of prolonged (and eventually painful) kicking to get the door open. I also managed to wake up all the neighbours, and it’s always fun to be the centre of attention …
Finally, the door gave and we gained access, we were greeted by the elderly woman sitting on the floor smiling at us – earlier in the morning she had fallen and couldn’t get up. When we had tried banging on her windows she had been asleep, and it was only the repeated bashing of my foot against her door that had caused her to wake up.
This was a good job in a number of ways: the lady was happy and healthy, and just needed a hand to get up off of the floor; I got to kick in a door and get away with not causing any serious damage; and finally we looked like heroes to the two daughters of our patient. There were smiles all round and we left the job feeling that we had really been of some use today.
Substitute
I know that the ambulance service is being used as a substitute GP service these days, but it really takes the biscuit sometimes. Take, for example, the job I was sent on last night. It came down to our ambulance as ‘Patient wants to kill his doctor’.
I immediately called up Control on the radio and asked if we were being sent because they couldn’t find the patient’s GP? Although I was half joking, I wondered what good we could do for the patient. Control got back to us, and let us know that they were sending the police, and that we should wait until they turn up. However, when we arrived at the address we knew who the patient was – so we cancelled the police and sorted out the patient’s problem.
I mention this if only because, when I got back on station and read the local newspaper, I found a story about a coroner’s investigation into the death of a 55-year-old female who had taken a fatal overdose of bloodpressure medication. When Control asked if she was violent, they were told that yes, the patient was violent. The police were called and the crew waited at a rendezvous point for half an hour until the police turned up. By then it was too late, and the patient died. Once more, the paper blames the ambulance crew. It doesn’t blame the psychiatric services who discharged her a few weeks earlier after a failed suicide attempt, neither does it blame the person who made the phone call that said that the patient was violent. It blames the crew who, quite rightly, waited for the police. If one of the crew had been stabbed to death, it might be a more sympathetic headline. We are expected to go into people’s houses, where we have been told that the patient is violent, where we could get assaulted or even killed – but as soon as we start thinking about our own safety, we are the ones to blame for anything that goes wrong with that patient.
Violence from the drunks, druggies and criminals doesn’t worry me – the job that worries me is the little old lady who has become confused and is sitting in her living room with her husband’s service revolver, or her favourite kitchen knife, desperate to stop the strange men in green from stealing her away in the night.
As normal the ambulance service has investigated, but in a show of support for its road staff, has stated that the policy of waiting for the police at a rendezvous point is the correct thing to do.
We are not cowards, but neither are we stupid/paid enough to wander into dangerous situations.
Nicked
I’ve just gotten on station for the start of my shift, only to find out that some scrote had broken into the station last night and nicked the video recorder and DVD player.
I mean, it’s not like we are ever on station long enough to use them, but it’s the principle …
These are the sort of people that we serve, these are the sort of people we are polite, professional and caring towards – and this is how we are repaid …
More Nicked
It’s getting so you have to tie things down now …
Yesterday a ‘Decontamination POD’ truck was stolen; this is an unmarked truck that we use to carry around chemical incident equipment. The current word is that this truck was carrying a load of atropine, which is the treatment for nerve agents.
If people were to start injecting this into themselves, they could get serious (as in fatal) effects.
I leave it as an exercise for the reader to decide if this is a good or a bad thing …
You Decide
Still no drunks, but the weekend starts today and my shift ends at 2 a.m. …
I’m going to describe a job I went to last night.
The patient is female and 30 years old. She is married and is attempting to get pregnant. The only medicine she is taking is fertility treatment, and she is (obviously) having unprotected sex; she is normally fit and healthy and has no allergies. Her normal menstrual period is regular, but her period is over 2 weeks late this time around. She has been having nausea and vomiting for the past 3 days. She has no abdominal pain, and is not tender or guarding. She has no pain or increased frequency of passing urine. All vital signs are within normal limits.
So … given this information …
(a) What do you think is ‘wrong’ with her?
(b) Does she need a trip to hospital in an ambulance?
(c) Why do you think she hasn’t done a pregnancy test?
Dragging
Sometimes a day can just drag along. Today, due to rather unusual circumstances, the day really dragged. Here is the time-line of today:
10:00 Turn up for work, brew a cup of tea.
10:01 First job of the day, taking someone from Newham hospital to Barts hospital.
10:02 Cut my finger on my locker door, try to stop bleeding, look for plaster.
10:23 Give up search for a plaster – there are none on the station – leave for Newham hospital.
10:26 Arrive at Newham hospital, ask for plaster; they also don’t have a plaster so I now have a huge dressing on my finger.
10:28 Meet with patient, pleasant woman – meet nurse who will be accompanying patient, barely understand nurse because of her inability to speak English.
10:30 Get patient’s notes and read them – they make more sense.
10:32 Ask nurse in charge why this patient (who is having cardiac monitoring and a blood transfusion) is going to an outpatient department. Get told that the patient ‘just is’.
10:54 After packaging the patient on a stretcher, loading them on the back of the ambulance, we set off for Barts hospital.
10:55 Nurse escort tells me that she gets travel sick.
10:55 and 20 seconds Give nurse a vomit bag.
11:37 Arrive at Barts hospital.
11:38 Enter outpatients’ department. Reception seem rather surprised to see patient on stretcher appear in front of them.
11:40 Problem is referred to the sister in charge, she also looks befuddled.
12:00 We wait while sister in charge phones around the hospital trying to work out why this patient is in her outpatient department.
12:30 Still waiting … We let Control know why we are waiting – there is no stretcher/bed to put the patient on.
13:00 Still waiting.
13:30 Still waiting – we let Control know that we still have the patient on our stretcher while they work out what they are going to do with our patient.
14:00 Still waiting.
14:30 Still waiting – we let Control know that we haven’t gone to sleep, we are told by sister in charge that patient will be admitted soon.
14:45 We place patient on an examination bed so that we can go back to answering emergency calls; patient will hopefully be in a hospital bed soon. We leave the nurse escort with the patient.
14:48 We are finally available for another job.
14:49 We realise we have nearly no fuel, and no fuel card to pay for fuel. We decide to return to station to borrow a fuel card off an unused ambulance.
15:20 We arrive back on station to look for fuel card (and have a cup of tea).
15:30 We leave to get fuel. Take infusion pump back to hospital – the ward seem surprised that the patient has been admitted to Barts.
15:48 We have fuel, we are now ready for another job.
16:00 We get a call, out of area Matern-a-taxi.
16:09 Arrive at Matern-a-taxi, contractions (genuinely) every 2 minutes, previous baby born in 3 hours, drive rather quickly towards her booked hospital.
16:12 Patient’s waters break – start swimming in back of ambulance.
16:20 Arrive at hospital.
16:24 Throw patient at midwife, run back to ambulance.
16:30 Tell Control that we need to return to station to mop out the back of the ambulance.
17:20 Get back to station, mop out.
17:45 Crew to relieve us are already on station; await ambulance to dry out.
18:00 Leave for home.
18:37 Get home, collapse into sofa, start writing this post.
- Fin -
This is how you get to work an 8-hour shift, yet only do two jobs …
After this post I got given a box of plasters by a fellow blogger. No more searching around ambulance stations for sticking plasters.
Sedation
I should be working today, but (and I want loads of sympathy here folks) I’m off sick with a work-related injury. Thankfully, it’s nothing too serious, certainly nothing as serious as last time when I swallowed HIV-positive blood.
On Thursday we got called to a big conference centre in town for a (possibly) suspended/dead/fitting male. We rushed over there and were met by their security who had rather cleverly staked out both entrances to this place so that they could lead us to the patient. Parking up we had to climb a couple of flights of stairs carrying nearly all the equipment from the ambulance. Our first-response bag, oxygen and associated kit, defibrillator, suction and carry-chair are quite heavy and, as we were in a rush to get up the stairs, we were a bit out of breath when we reached the patient.
The first thing that we saw (and were very happy about) was that the patient had not suspended, and was instead thrashing around on the floor with some security guards and the centre’s medic sitting on top of him. Approaching closer we saw that he wasn’t fitting, but was instead very combative, trying to fight off the people who were holding him down in a very confused nature. ‘Aha!’ we thought, ‘he’s post-ictal’.
During the post-ictal phase of a seizure, the fitting has stopped, but the patient is often disorientated, sleepy or aggressive. In this case it appeared that the patient was both confused and aggressive – he was not responding to anyone trying to talk to him to calm him down, and he could only make guttural sounds. Normally, these episodes last less than half an hour, so we stay with the patient until we can get them into the ambulance.
Sometimes the aggression can come from physically being held down – the patient is confused and frightened, and all they can feel is people holding them down, so they struggle. I suggested that the security guards let him go, which resulted in the patient trying to stand up, only to fall over again (don’t worry, we caught him) and unfortunately the centre medic got a head butt for his trouble. I managed to get a blood glucose reading, which was normal, and a work colleague phoned the patient’s mother, so I could get a bit of history. The patient is normally fit and healthy, not diagnosed with epilepsy, but has had 2 fits in the past 2 years. All during this phone conversation the mother could hear her son shouting in the background. He had never been violent before.
We resigned ourselves to a bit of a wait, so we managed to get him over to a leather couch, and held him down there. After 10 minutes there was no change in the patient’s condition – normally they get a bit tired or they start to have a change in their condition. So we started to think about other ways in which we could help the patient at the scene. We couldn’t get him to the ambulance while he was so combative, and so we thought he might need some form of sedation. I ran back to the ambulance and asked Control to get us a BASICS doctor, or at least someone who could give some form of sedation.
Instead after about 10–15 minutes we got the PRU (Physician Response Unit), which is a new service where a doctor from the Royal London Hospital covers medical emergency calls – it’s a bit like HEMS, only without the helicopter, and instead of going to trauma they mainly deal with medical emergencies.
The doctor (who is a very nice man) and paramedic crew with him took one look at the patient, listened to the history and decided that sedation was a very good idea.
Cut forward 40 minutes’ worth of trying to sedate the patient with increasing amounts of medication. For the medically trained out there, the patient needed 10 mg haloperidol and 17 mg of midazolam. At one point the doctor was thinking about knocking the patient completely out and intubating him. Luckily the patient was sedated enough for us to get him out of the conference centre and into out ambulance, where we ‘blued’ him into Newham hospital just in time for him to wake up (the sedation lasting only around 15 minutes) where the doctors there did paralyse and intubate him.
We have few ideas why the patient was so violent and so deeply confused – it’s something that will be investigated in hospital. We were considering epilepsy, head trauma (from when his head hit the floor), meningitis (so antibiotics were given on scene) or some form of brain insult. I’m asking my crewmate to find out what happened to the patient.
The reason why I am off sick? Well after holding the patient down for an hour and 10 minutes, I managed to sprain my thumb. Since I can’t be considered safe to carry a patient downstairs, I’m taking today off (plus 2 days of leave) so that my thumb can heal and I can get back to saving lives picking up drunks again on Monday. Oh, and it’s my birthday tomorrow – 33 is such a young age don’t you think?
I did manage to see the patient again … see the next entry.
Patient Gets Better!!!
I went to visit our patient from the last post. This morning I’d put my hand in my pocket and found that I had £2.66 of his money that had spilled out of his pocket during our struggle and I’d put it in my fleece for safe keeping – given the saga of the job, I’d forgotten to hand it in when we reached the hospital. I thought it would be best if I returned it to him, so I had a chat with the lovely receptionists at the hospital, and they told me what ward he was on.
I went to the ward to find him sitting there, seemingly none the worse for wear. He did have a bit of a black eye (not my fault … honest), and when I spoke to him he told me that the doctors suspected that he had fainted, and when he had hit his head had suffered a form of concussion. His CT scan and blood tests were all normal, although I suspect that they will be running EEGs (electroencephalograms) and other more detailed tests a little later. He told me that he was feeling pretty much normal and I suspect that they are keeping him in hospital to continue to run their tests.
He was very pleased to see me, and we had a little chat. I offered him his money but he refused and suggested that I get myself a pint with it.
It’s the first time I’ve actively gone to look for a patient after bringing them into hospital – and it is a weird experience going into a ward to see a patient whom I last saw trying to fight me. Yet another new thing I’ve done because of writing this blog.
Safety Net
I’ve mentioned before how the ambulance service and the A&E department are often seen as a ‘safety net’ by other health-care providers. Both yesterday and today we had perfect examples of this.
Yesterday we were called by a 70-year-old man with a urinary catheter which had blocked. This is a fairly simple thing to solve as it just needs a flush of water up the catheter to clear the blockage. It’s a 5-minute job that we, as ambulance crews, aren’t allowed to do. However it is the sort of job that district nurses are supposed to do.
So why hadn’t a district nurse been to see the patient so that she could flush the catheter and prevent the patient from having to attend A&E? Why was the patient, who had phoned up the nurse himself, and told her exactly what he needed doing, forced to call an ambulance?
Because the nurse didn’t have any water to actually flush the catheter. It’s a bit like if I turned up to someone having an asthma attack, and didn’t have any oxygen to give them.
So the district nurse told the patient to dial 999 for an ambulance. We arrived and found him with a bladder so full it was causing him severe pain. We took him into Newham hospital, who, within minutes, had cleared his catheter, and eased his pain. They gave him a ‘takeaway’ bottle of water so that the district nurse wouldn’t have an excuse the next time she needed to visit him.
Today, we were called to a patient who needed his anti-Parkinson’s disease medication. He had a carer, who was supposed to visit him once a day to clean and arrange his medication. But for the last 2 days, because the ‘carer’ couldn’t get in touch with the patient’s GP, she’d just left him without his medication. We turned up, not knowing what we could do to help. The flat in which the patient was living is brand new, and yet was already very untidy. The patient told me that he was lucky if the carer spent longer than 5 minutes with him (the carer is contracted to work with him for an hour a day).
This poor man was left, alone and shaking, with a carer who seemed to think that if she ignored this ‘problem’ it would soon go away. So, we did the only thing that we could: we took him to hospital, so that they could sort out his medication for him. Meanwhile I filled in an ‘LA260’ which is a ‘vulnerable adults’ form and allows the LAS to bring situations of abuse, and potential abuse, to the attention of the local social services. They now have the name of the care agency, and this problem can be solved before it repeats itself in a month’s time.
Hopefully, someone will get a bollocking, and our patient will get a carer who actually cares for him.
It often feels that we, and the local A&E departments, are left to do the jobs that other people should be doing, but because we are there, these other agencies don’t seem to care about doing a competent job. I’m aware that there are probably loads of health visitors/social workers/district nurse/CPNs and GPs who do actually give a damn about their patients – it’s just that we never seem to meet them.
I never did get any feedback from the LA260 that I filled in – normally you get a little note sent to you explaining what has been done to resolve the situation.
A Hidden Pregnancy
Our ‘interesting’ call of last night was a Matern-a-taxi. What, I hear you ask could be interesting about taking a pregnant woman 1.2 miles into the local maternity department?
Well, apart from the patient, no-one else knew that she was pregnant – she had been hiding the pregnancy from everyone. She hadn’t seen a doctor; neither had she booked into a maternity department. Her family suspected nothing. It’s not as if she were a ‘large’ woman, who could perhaps hide the tell-tale bump under the pretence of fat. She was actually rather slender, which leads me to ask how she could hide her rather obvious pregnancy from everyone.
When my crewmate spoke to her (I was driving), she told him that she had hoped that the pregnancy would ‘go away’.
We tried to prewarn the maternity department that we were coming (because she was quite close to actually delivering the baby), but they hung up the phone twice on our Control. The problem is that the entrance to the maternity department is locked at night, and we need someone to come down and open it for us. So … we were left standing around outside the department waiting for the midwives to phone for a porter to traipse the length of the hospital to come and open the door for us (as opposed to one of the midwives walking down the stairs and opening the door).
By the time we got in the patient was starting to bleed, and we were getting more irate at the apparent ignorance of the midwives.
So, tonight we are going to put in a ‘clinical incident report’ to highlight the danger that standing outside the maternity department for 10 minutes while they arrange a porter puts the patient in.
One of the people on complex has had to deliver a baby in the back of their ambulance while they were waiting for the doors to be opened, so something needs to be done.
Upsetting
Three of our jobs today had the potential to be upsetting, and while they were all sad, only one seriously upset me, and did so in a way I consider rather out of character for myself.
The first job of the day was to an 86-year-old female in a nursing home with a ‘blocked nose’: we raced around there because … well … it was a Category ‘A’ call and those are the top-priority ‘get there in 8 minutes to please the government target’ calls.
Just as we pulled up outside Control let us know that the patient was upgraded to a ‘Suspended’ (no pulse, no breathing), and sure enough we ran into the home to be greeting by a FRU who was doing CPR. I jumped down and did a round of chest compressions, which cracked her ribs (a recognised side-effect of effective CPR), and then noticed that on the cardiac monitoring machine her heart rhythm had changed. She had a pulse! … People don’t normally get a pulse back from cardiac arrests of her particular type. We rushed her to the hospital, where a full cardiac arrest team was assembled. Her pulse was lost, and then returned. Unfortunately, her prognosis was poor, but she stayed alive long enough for her daughter to reach the hospital. She died with her daughter there, which is a small victory, but one that we are getting more used to.
The second potentially upsetting job was to a 1-year-old boy who had pulled some boiling milk on top of him. We turned up to find about 20 police officers on scene, and the HEMS helicopter circling above. The same FRU responder was there and the child had around 10% partial thickness burns to parts of the neck and chest. While nasty, this wasn’t immediately life-threatening, but the HEMS doctor who turned up decided that it would be best to take the patient to the Paediatric Burns Unit at Chelsea and Westminster Hospital by helicopter. As the helicopter could get the child there in under 20 minutes it seemed like the right plan of action. My job during this call was to (1) hold onto the other two toddlers in the house, (2) mix up some paracetamol for the child, and (3) drive child and doctor to the helicopter, which was around 300 yards away. The job was interesting because she was the type of parent who thought it was a good idea to wedge a settee into the hallway to stop her children from falling down the stairs …
The final job was a lot simpler – we were called to an 18-to 22-year-old female who was ‘unresponsive’ in a bus. The bus had reached the end of its route and the driver couldn’t wake up the patient. (Possibly interesting aside – bus drivers cannot touch any of their customers to wake them up.) We turned up and soon managed to wake up the very sleepy girl. She remained drowsy but agreed to let us take her to the place where she lived, but after talking to her a bit, we soon realised that she was homeless. This, coupled with the way she would fall asleep as soon as we stopped talking to her, made us think that it would not be safe to leave her on the street. We decided instead that we would take her to hospital. When we reached the hospital she refused to go in, and instead pulled out a ‘crack’ pipe and started to light up. We told her that she couldn’t do that … So she jumped up, pushed my crewmate and ran off. As there was nothing physically wrong with her we couldn’t chase after her; instead we returned to our station to fill in the necessary paperwork.
So why was it that this last job was the most upsetting, not only for myself but also for my crewmate? Well it wasn’t because she was pretty (she wasn’t, and she had a remarkably nasal voice), and it wasn’t because she was ill, neither was it because my crewmate got shoved.
With our first job, the woman was at the end of her life, and until she died, had enjoyed fairly good health. She didn’t die a painful, protracted death, and she died with her daughter next to her. With the scalded child, he would forget the pain, and will receive excellent care from the hospital he went to, he would return home to his loving (if ever so slightly dense) mother. With this girl, it was as if she were lost; at some point in her life her potential future had unravelled. Instead of getting an education, holding down a job, finding someone special and living a long and happy life, she is homeless, a drug addict, and her future is probably painful and short. What is so depressing is that no-one was able to turn around this descent, and this is perhaps why I despair at society – that so many people are prevented from reaching their full potential. I understand that she has made her own choices, but how much power did she have to make those choices? I wanted to help her, but there was no way I could do this.
And it’s that which annoyed and upset me.
I keep getting upset and annoyed at the same things – the waste of a life is a terrible thing to see. That, and the knowledge that I am helpless to do anything to change it. I imagine that this is why I dislike alcoholics so much.
Therapy?
We got sent to a job of a 6-month-old baby not breathing. While this often means that baby has a cold, it could also be one of the worst jobs you can get. We sped to the address and entered a house where the whole family was distraught. It was an Indian household, so there were a lot of people there, and most of them were crying. Once more, I heard the type of crying that can only mean that something awful has happened – entering the living room I instantly saw a baby lying dead on the settee, father crouched over it crying and the mother standing and wailing, shouting out that her baby was dead.
There is only one thing that you can do in a situation like this, which is to scoop up the baby and run to hospital as quickly as possible. I reached down and picked up the baby; I was shocked to find that it was as stiff as a board and very purple, indicating that it had been dead for some time. It looked more like a doll than anything that had once been alive. We could have recognised the child as dead on the scene, but taking the child to hospital would mean that the parents would see that everything that could be done was being done and, more importantly, they would be in a hospital with all the support that the hospital could provide.
I ran out to the ambulance with mother in tow, and told my crewmate to get us to hospital as quickly as possible. The father and grandmother followed behind us in another ambulance who had heard this call go out and had turned up to see if there was anything that they could do to help. On the way to hospital I did the CPR that I knew was ultimately pointless and spoke to the mother. She had last seen the child alive at 3 a.m., and he had been fine then. It looked like it may have been a case of sudden infant death syndrome, and I did all that I could to prepare the mother for the worst.
We pulled up at hospital and handed the baby into the care of the hospital. I spoke a little more with the mother and grandmother, but there is nothing that you can say to people who have had such a tragedy. Our station officer met us at the hospital and asked us if we were alright, then he booked us off the road so that we could go back to station and have a cup of tea and ‘decompress’. If we needed more support I think it would have been there, but I just wanted to get away from the hospital.
I’m not often affected by jobs, and this isn’t the first dead baby that I’ve had to deal with, but it is the first dead baby I’ve had since joining the ambulance service and it is very different from dealing with them in hospital. Going into someone’s house to take away a dead child is very different from having the child and parents turn up at hospital, which is your safe territory.
At the hospital all the other crews were asking if I was alright and, to be honest, I wasn’t really alright – I was upset that while I was doing CPR on the baby its legs were seesawing into the air, and it looked too much like a doll. There was a point after the job where I thought I was going to start crying, but a moment outside the Resus’ room and I was back to functioning as I normally do. I’m not weak, and when in the midst of something I can deal with anything – it was only after the doctors and nurses at the hospital had taken over that I started to feel anything.
We returned to station, where the therapy of talking about anal surgery with another crew, and a cup of tea, soon had me feeling better. It used to be that you would return to work straight after a job like this, but then I think they realised that if we got our normal inappropriate call (bellyache for 2 weeks sort of thing) we might say something to the patient that we might later regret.
Well, an hour on station later and I feel fully prepared to deal with that sort of thing again – but I think that I’ll be haunted by the image of that child lying dead on my trolley.
I had loads of people commenting on this post, loads of support, which was very much appreciated. The title is a reference to the fact that I have found my blog to be ‘therapy’ for some of the things that I’ve seen and done in the ambulance service … and it’s cheaper than hitting the bottle.
Dog Teams
I’ve often mentioned that the ambulance service and the police tend to get on rather well together; this is at least in part due to us both being called to the same jobs, and probably because we share the same view of the ‘Great British Public’.
An example: we got called to a drunk who was being verbally abusive to a bus driver – we were called because the drunk had fallen over, while the police were called because of the abuse. The drunk man was obnoxious, and well known to both of our services, and because of the lack of an injury was left in the care of the police. If he had been injured then the police would have left the matter in our hands.
So, when we co-respond, the ambulance crew pray that the patient is uninjured, so the police have to deal with them, while I suspect that the police hope that the patient is injured so they don’t have to arrest them.
However, there are a lot of specialist teams in the police service that we tend not to come into contact with that often; we mainly get to meet the normal ‘beat’ coppers. Thankfully, we rarely see the murder, child abuse, drugs or dog teams. This isn’t to say we never see them (and our station did get a Christmas card from the local murder squad telling us to ‘keep up the good work’), it’s just that it is fairly rare.
So, it was rather surprising that I met with the dog-handling team twice last week. On the first occasion, we were called to a known schizophrenic who had threatened to kill herself. The patient herself (a regular attender at the local A&E) was a bit of a pain to deal with, she wanted to stay at home and kill herself and couldn’t see why we wouldn’t let her do that. Her dog, on the other hand, was a real pleasure – happy to see us, interested in smelling all our equipment and extremely friendly. As the police were already there, they got the dog squad to look after the animal until the patient was discharged from hospital.
In case you think I am being harsh on the mentally ill, the patient attends A&E every day with the same complaint of wanting to kill themselves … she hasn’t managed it yet.
The second time I saw the dog-handling team was when we had to gain access to a house where the patient was unable to come to the front door and let us in. The interesting part in this story is that there were five dogs of unknown temperament in the house. For half an hour the police unsuccessfully tried to gain access, mainly by climbing up a ladder and trying to open a bathroom window. We were able to talk to the patient, and so we knew that they were not badly hurt, otherwise we would have had to kick the door down. Then the dog team turned up and, using a top secret criminal technique, managed to get the front door open in about 10 seconds, thus putting to shame the half-hour everyone else had spent trying to gain entry.
All five dogs were really lovely, although energetic, and at the end of the job I had to spend 20 minutes brushing the dog hair off my uniform.
There is a joke we have about dogs. When we ask a patient if the dog is friendly, the patient always answers that they won’t bite; the reply to this from the ambulance crew is to add the unspoken ‘They only bite people dressed all in green.’
I’ve only had one dog take a dislike to me. But I managed to pull my hands away from his gnashing teeth before he could catch me.
Perils of Drinking (Number 1 in a Series of 230)
It was the usual type of busy last night – we heard rumours that there is such a thing as an ‘ambulance station’, a mythical building where one might use the toilet or partake of the life-giving ‘cup of tea’. It must be a myth, as we never saw it at all.
As I have mentioned, we get our calls sent down to a computer screen in the ambulance cab; sometimes you wonder how the Control crew have entered it while keeping from laughing down the phone at the patient. A case in point was one of our calls last night which was given as ‘53-year-old male, taken 3 × crack cocaine, cold and lonely, needs to be put back together’.
Avoiding the rather obvious ‘Humpty Dumpty’ jokes, we soon realised that the complaint, and the location he was calling from, fitted one of our semi-regular callers. By the time we got there he had left the phone box and neither us nor the police could find him after a search of the area. Obviously I was distraught …
Our other stand-out job of the night was a 57-year-old male fitting. We quickly made our way to the location, to be met by a block of low-rise flats that often sneak up on you in our area. These are three or four floors high, and have no lifts. Also there was one of our First Responders. We entered the block, and immediately made our way to the stairs (it is a little known law of physics that in flats with no lifts, people on the ground floor are never ill … only those on the top floor).
Entering the flat, the general state of disrepair, mess and the 3-litre bottle of strong cider I tripped over tended to give the impression that it was owned by an alcoholic. We got into the living room to find a large man lying senseless on the floor, while his daughter was sat over him stroking his hand, trying to reassure him. A quick check over, some oxygen and a chat with his daughter revealed a history of alcoholism (surprise!) and the occasional alcoholic fit. He was a big man, so we packaged him up in our carry-chair and carried him down three flights of stairs. All the time his daughter was saying how strong the nice ambulance men were – which only goes to show that she wasn’t paying attention to my reddening face and struggles for breath …
We got the patient into the back of the ambulance where he started to fit again, this time lasting about 2 minutes. He also decided to bite his tongue and vomit, which meant that the back of the ambulance (and myself in some part) was covered in bloody, cider-smelling vomit. I think I’ve mentioned before how I can’t smell alcohol on someone’s breath, yet I can smell cider when it has been vomited all over my ambulance … and it turns my stomach. We packaged him up and ‘blued’ him into Newham, where he had another two fits (despite some rather strong sedation) and by the end of our shift he was still in Resus’ having infusions of phenytoin and Pabrinex.
So, a busy night without the chance to see our station, with at least one mopping out of the ambulance … pretty standard really.
The vomit in the ambulance took place at the end of our shift, so we couldn’t even get back to station to use the mop. Unfortunately, with the increased number of calls we have, getting back to station is becoming rarer than ever.
Security
Yes, I know I’ve written before about kicking down doors. However, in this post I offer people advice in making the beating down of their door as hard as possible. So please excuse the repetition. Like all good health-care professionals I regularly ignore my own advice.
There is a visceral pleasure in kicking down a door. Once or twice I’ve managed to see someone who is really ill trapped behind a locked door, occasionally there has been someone who has just been unable to open the door. And just the once I have kicked down a door that the patient refused to open because they were schizophrenic and didn’t want to open the door – not that I knew that at the time.
I’ve even been surprised at the ease in which I can kick down the doors of the flats that I live in. Actually, it would be more accurate to say that I am scared with the ease in which the doors can be broken. Oh well, it’s not as if I have a lot to steal anyway …
My experience of kicking down doors has taught me which security features are useful when trying to prevent someone from stealing your TV and video.
If you have a deadlock-type lock, then use it – always. The skill of kicking down a door relies on breaking either the lock, or the wood holding the lock; deadbolt-type locks are a lot more secure than the normal Yale type lock.
If you are in the house and have a bolt on the door, then use it. It takes a lot longer to kick down a door when there is a bolt in the way. Another trick behind kicking down a door relies on applying the force of your kick to the (hopefully) single point of resistance. If there is a bolt at the top or the bottom of the door it makes it a lot trickier to break that door.
Windows in the door are a bad idea – they are a weak point that can be easily broken, and then a skinny hand can reach through and unlock the door.
If you really want to be safe then have a bar across the door. I’ve seen it once or twice, and if someone has a bar across the door then there is no way I’d be able to break that door down. Just make sure you don’t collapse behind it.
Major Incident Cover
One of the perks of this job is the need to cover football games. Well … it’s a perk if you enjoy seeing your local team play. Personally, I can’t stand football but overtime is overtime, and it does make a nice change from the usual jobs I go to. So, this Sunday I got to see West Ham play against Derby.
The LAS provide ‘Major Incident’ cover for these games, we don’t look at sprained ankles or minor injuries (that is the job of the St John’s ambulance). We also don’t look after the players who get hacked down and are unable to walk, only to watch them turning somersaults a scant 5 minutes later when their team scores a goal (that is a job for the private medical firms).
So, unless a stand collapses, there is a major fire, a bomb goes off or someone drops dead in front of us, there is very little we have to do. At the West Ham ground (my local football club), there are four ‘road crew’ present, along with at least one major incident support vehicle, one radio operator and an officer. The road crew sit down near the pitch, while the officer and radio operator sit in a VIP box overlooking the whole ground.
Today I was given the role of ‘safety officer’, which doesn’t mean I’ve been promoted, it just means that in the event of a major incident, I’m supposed to watch out for the safety of the ambulance crews present, liaise with the police and fire service about any hazards that might be a problem, and to make sure that any crews that attend the incident are not getting too stressed. I also have to talk to the person in overall control at the incident about any issues within this sphere that may occur.
We were warned that there was an increased chance of violence at this match because some hooligan ‘supporters’ were appearing before the magistrate tomorrow, and that some of their ‘crew’ might want to cause some trouble. Luckily for us, that did not happen, despite a 2–1 loss.
It was really cold down there in the stands, I had my undershirt, shirt, body armour, fleece and hi-visibility all-weather jacket on, but I was still freezing. Anyone listening carefully as I walked around trying to keep warm would have heard a clink-clink-clink-clink sound as my frozen balls knocked together.
As I’ve mentioned before, I’m not a huge fan of football (overpaid idiots, getting more money in a week than I get paid in a year for booting around a plastic ball), so I spent most of the match listening to music (The Magnetic Fields) on my smart-phone, while stamping around trying to get some sensation back in my toes.
As a quick aside, who needs an iPod Shuffle? My smart-phone can do the same thing and more – it can even make phone calls …
Half-time came and went so we joined the St John’s Ambulance for a cup of tea and a sandwich, rather than watch a bunch of scantily clad young women prance about. Then we were back in the cold, where I tried to stay awake while West Ham, perhaps predictably, lost …
With the exception of someone having a crafty cigarette and setting off a fire alarm, it all went rather smoothly. I did find it funny that the people in the stadium knew what the ‘Inspector Sands’ announcement meant, and did nothing but laugh quietly at it.
At the end of the match we have to stay around until we are ‘stood down’ as the last few supporters leave, so we sat in the ambulance, with the heater going, wrapped in our own blankets (remember, we know what those blankets have been wrapped around, yet we still used them – that is how cold it was).
We then started making our way back to station …
… to come across a policeman who had tried to stop a car – only to have them speed up (possibly accidentally) and hit him. He wasn’t especially badly hurt, but we took all precautions as we transported him to hospital. He’ll need a few X-rays, but I suspect that he will be fine.
‘Inspector Sands’ is a codeword for use over a public address system. It is used to let the staff know that a fire alarm has gone off without alerting the public and possibly panicking them.
Phonetic
Конец ознакомительного фрагмента.
Текст предоставлен ООО «ЛитРес».
Прочитайте эту книгу целиком, купив полную легальную версию (https://www.litres.ru/tom-reynolds/the-complete-blood-sweat-and-tea/) на ЛитРес.
Безопасно оплатить книгу можно банковской картой Visa, MasterCard, Maestro, со счета мобильного телефона, с платежного терминала, в салоне МТС или Связной, через PayPal, WebMoney, Яндекс.Деньги, QIWI Кошелек, бонусными картами или другим удобным Вам способом.
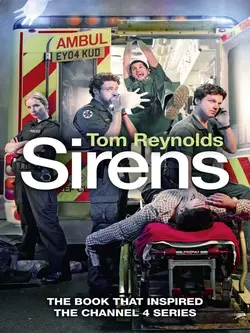
Tom Reynolds
Тип: электронная книга
Жанр: Биографии и мемуары
Язык: на английском языке
Издательство: HarperCollins
Дата публикации: 19.09.2024
Отзывы: Пока нет Добавить отзыв
О книге: Collected in one volume, here are the true life stories of London ambulance driver, Tom Reynolds.*Previously published as Sirens, after the Channel 4 TV show inspired by the book*On any given day Tom Reynolds might be attacked by strangers, sworn at by motorists, puked on, covered in blood and other much more unpleasant substances. He could help to deliver a baby in the morning and witness the last moments of a dying man in the afternoon. He deals with road accidents, knife attacks, domestic violence, drug overdoses, neglect and suffering.And you think you’re having a bad day at work?His experiences spawned two volumes of memoir, both of which are collected here.